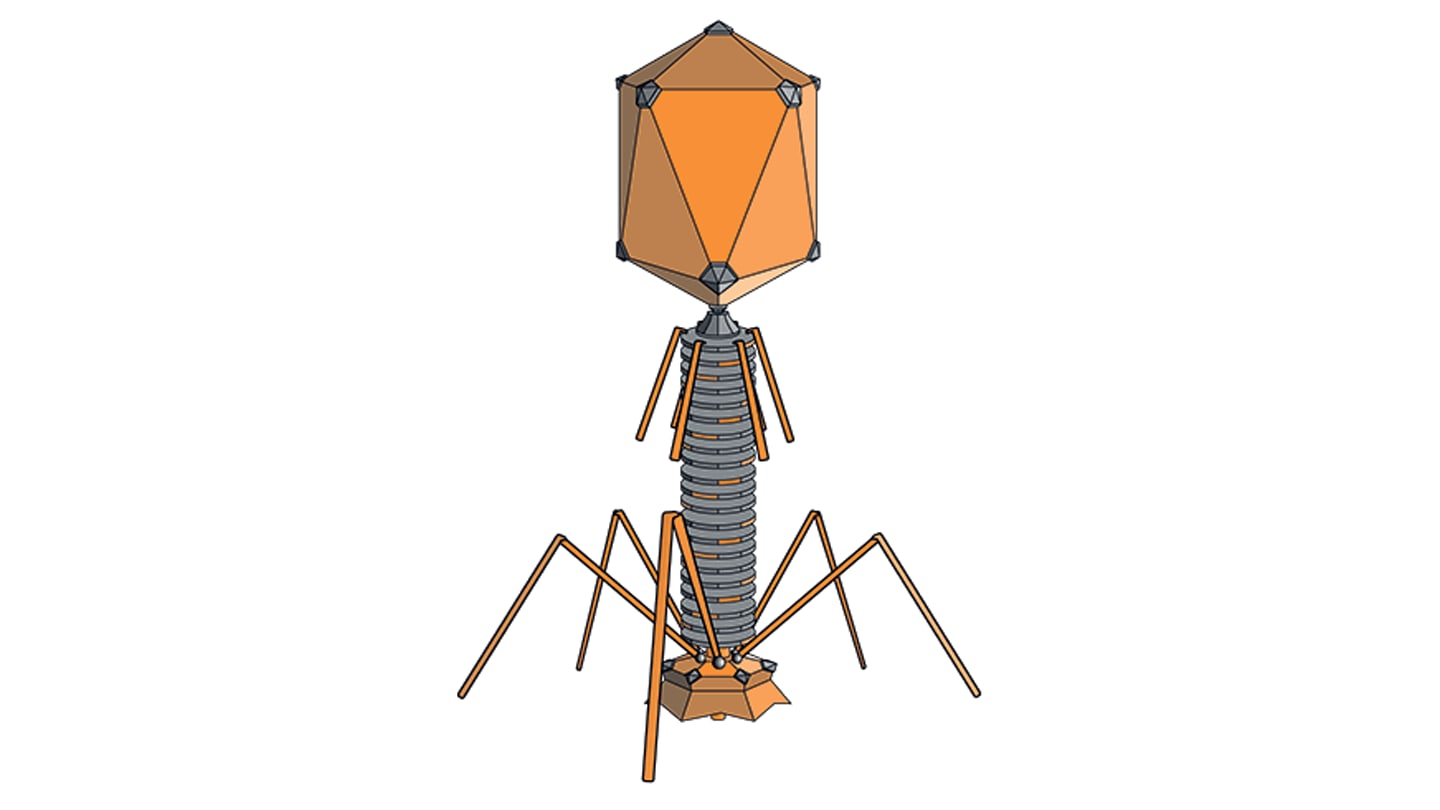
Researchers at the University of Bath, UK, have developed a technology that could enable protein-based drugs – such as antibodies, hormones, and peptides – to be administered orally rather than by injection. Protein medications currently require injection because they are broken down in the stomach. The new system, developed by the team of Randy Mrsny of the Department of Life Sciences, employs a technique that mimics a natural bacterial mechanism in the gut. A therapeutic protein, demonstrated in the study using human growth hormone, is linked to a non-toxic carrier derived from a bacteria related to cholera. This carrier binds to receptors on intestinal cells, ferries the drug across the gut wall, and safely releases it into the bloodstream without damaging the epithelium.
In vivo experiments consistently delivered between five and 10 percent of the drug into the bloodstream – an efficacy considered commercially viable. The research, published in the Journal of Controlled Release, indicates potential applications for therapies in growth hormone treatment, cancer immunotherapy, and metabolic drugs like Wegovy and Ozempic. With work now underway to refine the method, and human trials on the horizon, we spoke with Mrsny to learn more about the origin of the concept, as well as what comes next.
What inspired you to pursue orally available protein-based drugs?
Our research focuses on gaining a deeper understanding of events that control health and disease in two of the body’s organ systems that constantly confront the outside world: the respiratory tract and the gastrointestinal tract. As part of our research, we explored how pathogen-derived toxins can enter the body by traversing epithelial cells lining the surfaces of these organs by hijacking specific elements used by these cells in their normal function. Recognizing the opportunity to deliver biopharmaceuticals using these same pathways led to a whole new area of research that has now allowed us to deliver these therapeutic agents in ways that could improve convenience and compliance for patients living with chronic conditions. Thus, our inspiration came from observing Mother Nature to examine how pathogens overcome epithelial barriers in the gut that limit the systemic delivery of biopharmaceuticals following oral dosing.
What setbacks did you face, and what drove you on?
There have been inevitable setbacks in our efforts to translate this approach. Many of our research grant applications were rejected; often from concerns related to previous efforts in this field where strategies were used to overcome the intestinal epithelial barrier by physical damage. As repeated damage to this barrier is a justified concern, we took additional efforts to clarify and demonstrate that our biological approach did not result in damage to epithelial cells lining the small intestine. Oral protein delivery has not been a priority of academic funding schemes, directing us early on to venture funding support to demonstrate the feasibility and safety of this strategy. In hindsight, this turned out to be very important as we could align with people who had a shared vision and financial capacity required for clinical testing. A belief in our biological approach, obtaining validating experimental data, and having an appreciation of the impact our work could have on improving patient care, was what drove us on during difficult times.
How did working on this topic shape your perspectives beyond academia?
After my postdoctoral studies, I began my career in industry, working at biopharmaceutical/biotech companies, focusing on basic research for the advanced delivery of their products. The years I spent in industry gave me an appreciation for the multiple, interconnecting components of the complex drug development pathway. On returning to academia and focusing on the technology, I am now helping to take these experiences forward. The experience enables me to see all aspects of translational efforts and the strategies used to mesh activities from one domain with another for the efficient and effective translation of a novel drug delivery approach – from basic biological sciences to applied pharmaceutical and clinical sciences.
What are the most significant scientific or technical hurdles that still need to be addressed before this approach could reach clinical trials?
Our basic biological pathway strategy was shown to be safe and effective in clinical phase II studies for oral delivery through studies performed by a company I founded some years ago. That technology was based on a chimera composed of a bacterial-derived carrier element genetically coupled to a protein therapeutic. I designed that molecule to efficiently transport across the small intestinal epithelium and to remain within the lamina propria, the tissue compartment located immediately below the intestinal epithelial barrier. This strategy allowed us to obtain an initial safety and efficacy proof of concept for our biological approach through phase II, as well as validation of scalable production and tableting processes.
Our bigger goal, however, was to deliver a therapeutic protein to the rest of the body. To achieve this, we needed to find a method of efficiently separating the carrier from the therapeutic protein cargo after its transport across the intestinal epithelium. Efficient carrier-cargo separation has now been achieved by our identification of a human carrier, Transcellulin, to replace the bacterial-derived carrier used previously. As we have now demonstrated this systemic delivery outcome, our next big hurdle is to validate it in the clinic. With our previous clinical success (and having identified a novel humanized carrier-cargo separation mechanism that works in human intestinal models in vitro), as well as experience with producing tablets, we feel there are no significant scientific and technical hurdles remaining for us to enter clinical trials.
Which target indications have you identified?
We are now looking for a pharmaceutical partner to demonstrate the safety and efficacy of our novel separating carrier/cargo chimera technology for systemic delivery to treat obesity and diabetes, short stature in children, or monoclonal antibodies for treating chronic diseases and cancer. Our strategy will be to work with a few selected partners to identify and focus our technology on high probability successes for an impactful clinical indication.
What kind of partnerships or collaborations would be critical to move this work forward?
By partnering with established pharma companies, we will have access to their extensive expertise and infrastructure in manufacturing, regulatory, and clinical trials. We need to remain intimately involved in these programs because we provide extensive and unique experience making oral dosage forms for delivery of a protein drug. Part of what we bring to such partnerships is our understanding of unique pharmacokinetics and pharmacodynamics inherent with oral delivery of biopharmaceuticals that could likely be distinct from systemic dosing in certain cases.
What outcomes would be the most meaningful?
We are very excited about being on the cusp of demonstrating a technology based upon a natural biological mechanism of the human small intestine capable of efficiently and consistently delivering a protein therapeutic to the systemic circulation following oral administration. Oral dosage forms to achieve systemic protein delivery can be easily produced using well-established tablet production and enteric coating technologies. Thus, we are excited about the prospect of developing a platform technology that could be cost-effective and generally available to patients.