Accepting R&D Failure
To file, or not to file – that is the question when it comes to IND applications. Companies don’t always make the right choice, but learning when to abandon ship can open the door to potential future gains.
Admitting defeat in pharma R&D and terminating a failing project is a hard decision to make – and sometimes companies file for an Investigational New Drug (IND) application despite unpromising data. Why? A group of researchers recently asked this very question and decided to publish an article on the subject to highlight the issue (1). We spoke to one of the authors, Dennis Lendrem, translational research project manager at the University of Newcastle’s Institute of Cellular Medicine, about the problems facing R&D.

What inspired your interest in this area?
In 1990, one beautiful sunny spring morning, I flew down to Heathrow for a meeting at corporate HQ to discuss the fate of our latest, brightest drug candidate.
The question? To file, or not to file, the IND?
The data did not look great. The debate that day hinged around whether we needed additional toxicity data to submit. The argument for immediate submission was that additional toxicity data would delay the IND and might even yield further negative data. In my mind, it was a no-brainer. We might not need the additional toxicity data to submit, but we needed to know whether we were storing up trouble later down the line. We should either drop the project right there and then, or run the additional toxicity study. Whether we met our IND quota for the year was irrelevant. Truth-seeking is more important than progression-seeking – at least in my opinion…
Why is it hard to terminate failing projects?
It isn’t. It requires brutal, pathologically objective, rational decision making. But decision makers are human and there are powerful cognitive biases at work here – hindsight bias, confirmation bias, optimism bias and narrative bias. These, coupled with the simple heuristics shaped by our evolutionary history, mean we are dominated by loss aversion. This gives rise to problems such as the “sunk-costs” fallacy, where we fail to terminate projects in order to avoid losing monies already lost. There are strategies to avoid such biases. These strategies can be learned. But they must first be taught.
Are we facing a crisis in R&D productivity?
R&D productivity is low; late-stage attrition is high, and drug development is costly. Much of the development costs are those associated with unmarketable drugs. For most drug candidates, the ultimate customer is the wastebasket. If we accept that most drugs in our portfolio are unlikely to see the light of day – and that most will end up in that wastebasket – it allows us to focus on terminating faltering projects as quickly and efficiently as possible. By terminating unmarketable drugs fast, we free up resources to develop more promising candidates.
How has the problem escalated?
Some analysts believe the industry has turned the corner and is on the comeback trail, but these analyses are deeply flawed (2). The problem escalated rapidly between 1990 and 2010. During this period, ‘development speed’ initiatives inadvertently sub-optimized the entire drug development process. At the time, development-speed thinking seemed attractive. If you want to increase R&D productivity, then reduce cycle time. What could be simpler? The industry set about re-engineering its development processes to maximize development speed. And the industry was remarkably good at doing this. By carrying out development tasks in parallel, we were able to rapidly speed up the development of these successful drugs. And by 2010 the cycle time for successful drugs had halved.
But we forgot that most drugs are not successful and never make it to market… so in reality we became really slick at delivering late-stage failures to the marketplace. And by placing tasks in parallel, we simply increased the burn rate of R&D. The cost of terminating drug candidates increased drastically. That cost must be borne by those drugs that do make it to market.
The Seven-Point Plan
Are the industry’s ‘quick-kill’ R&D strategies efficient?
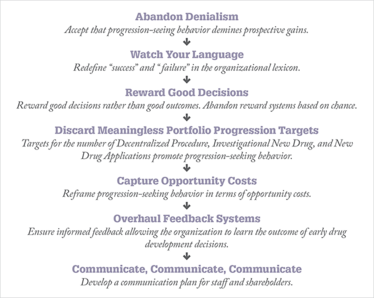
There is no question that ‘quick-kill’ is more efficient than traditional strategies. Quick-kill is about building opportunities to terminate candidates earlier in the development process. Sometimes this involves a profound understanding of the operating characteristics of existing tests. Sometimes it involves the introduction of assays that may (or may not) be part of a regulatory submission. So there are technical challenges in developing these assays and understanding their performance. However, in working with organizations, we found that the real challenge is the cultural and organizational attitudes to quick-kill. Hence, we’ve developed a Seven-Point Plan. For me, the key is to capture and communicate the opportunity costs of progression-seeking behaviour – and to reframe termination decisions as prospective future gains.
As you’ve researched this area, what are the most worrying findings?
Complacency. Complacency will be the death of many large, pharmaceutical companies. Many do not accept the need for change. The larger and more successful the corporation, the greater the denialism – and the greater the inertia to make changes to ensure their future.
The current draconian efforts to stem rising R&D costs are unlikely to lead to sustainable R&D productivity improvements. Meanwhile, we flail around grasping for quick fixes to problems that we don’t have. We are rearranging chairs on the deck of the Titanic.
I guess it’s easy for us here in Newcastle, UK, because we are sitting on industry estimates of the false positive and false negative rates at each stage in the drug development process. These estimates will be published before the end of the year. Once in the public domain, they will allow pharmaceutical executives to estimate the opportunity costs of progression bias and late stage attrition in R&D. And the industry is in for a shock…
- Richard W. Peck et al., Nature Reviews Drug Discovery, doi:10.1038/nrd4725 (2015).
- Dennis Lendrem et al., Pharm Stat., 14(1), 1-3 (2014).

Making great scientific magazines isn’t just about delivering knowledge and high quality content; it’s also about packaging these in the right words to ensure that someone is truly inspired by a topic. My passion is ensuring that our authors’ expertise is presented as a seamless and enjoyable reading experience, whether in print, in digital or on social media. I’ve spent fourteen years writing and editing features for scientific and manufacturing publications, and in making this content engaging and accessible without sacrificing its scientific integrity. There is nothing better than a magazine with great content that feels great to read.



















