
Choice Matters
A mosaic-based vaccine could offer at-risk people more choice when it comes to HIV prevention.
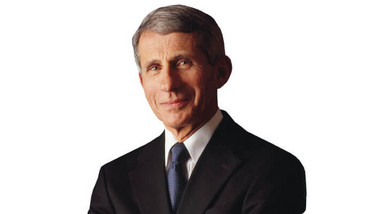
Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases (NIAID) at the US National Institutes of Health.
Antiretroviral drugs have helped transform HIV from a life-threatening infection to a manageable chronic condition – an advancement that was almost unimaginable in the early 1980s. When Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases (NIAID) at the US National Institutes of Health, first entered the field, the disease didn’t even have a name, but he recognized the potential ramifications for the global community. “In 1981, I was in the early stages of a successful career studying immune-mediated diseases when the first reports came out describing the disease that would later become known as AIDS. I recognized very early on that this was going to become a global problem, and I decided to switch my focus and begin researching this disease that did not even have a name at the time – much less a known etiology. That choice informed the entire trajectory of my career,” says Fauci, whose vast research portfolio has resulted in substantial contributions to the ways HIV/AIDS is prevented, diagnosed and treated today.
Though there are more than 30 highly effective antiretroviral drugs, as well as a wide array of non-vaccine prevention strategies including PrEP (a daily medication taken by those without HIV to reduce their chances of acquiring the virus), these solutions alone are unlikely to bring about a durable end to the HIV pandemic; vaccines are a much-needed addition to the current prevention toolkit.
Fauci and NIAID have been working with the HIV Vaccine Trials Network, the US Army Medical Research and Development Command, and Janssen on the development and testing of a “mosaic-based” vaccine for HIV, which is made up of elements from different HIV subtypes and uses Janssen’s AdVac adenovirus vector platform. It is administered through four vaccinations over the course of one year. It is hoped the two-vaccine regimen will induce immune responses against a wide variety of global HIV strains, including both common and rarely-occurring strains of the virus. The newest study, Mosaico – a Phase III trial – will commence enrolment later this year at multiple clinical research sites in North America, South America and Europe, and will test the efficacy of the vaccine in 3800 in men who have sex with other men and transgender individuals.
A Phase IIb trial (known as Imbokodo) is also currently underway evaluating a mosaic-based HIV vaccine regimen in around 2600 young women, aged 18–35, across five southern African countries.
HIV is challenging from an R&D standpoint because there are no documented cases of people with chronic HIV developing a natural immune response that completely cleared the infection. Enrollment for clinical trials can also pose challenges due the cultural stigmas associated with HIV and sexuality.
“Despite the many valuable scientific advances in HIV prevention, optimal implementation of these modalities has been impeded by numerous structural and social barriers, including HIV stigma,” says Fauci. “People need choices for HIV prevention methods that meet their needs and fit into their lives, and NIAID is committed to developing and improving tools and methods to prevent HIV in diverse populations around the world. Our track record in engaging local communities during protocol development and prior to enrolling populations at high risk for HIV enables us to work together with them to successfully implement pivotal trials.”
Initial findings from Imbokodo and Mosaico are expected in late 2021, and 2023, respectively.
After finishing my degree, I envisioned a career in science communications. However, life took an unexpected turn and I ended up teaching abroad. Though the experience was amazing and I learned a great deal from it, I jumped at the opportunity to work for Texere. I'm excited to see where this new journey takes me!



















