A Chip Off the New Block
In vivo animal models have brought much to the science behind the drug development industry, but how far behind are organ-on-a-chip models for predicting human biology?
Tomasz Kostrzewski | | 3 min read | Discussion
The primary purpose of preclinical models is to predict human responses. Ultimately, more predictive models can better inform preclinical decision making, which in turn leads to greater success in clinical trials. Enter new methodologies such as organ-on-a-chip (OOC), which are designed to more accurately model actual human biology. By culturing human cells together to form microtissues, we can study responses from cells that use the same transporters, enzymes, and pathways as in humans, which allows us to reliably predict both the positive and negative interactions of a drug during preclinical research.
For a long time, animal models have been the main method of preclinical research; indeed, there is a great deal of literature and historical evidence to demonstrate their utility, which makes some people hesitant to transition to alternative methods. Animal models offer a complete system, including multiple organs, blood flow, and immune responses, and there is also a lot of existing infrastructure available to support these studies. But animals are not humans. Rodents, for example, have completely different metabolic and immunological systems to humans, which means they can be very poor predictors for various human effects.
In my view, OOC technologies are more convenient and significantly lower cost than animal studies. Because of the human-relevant data generated, researchers can use OOC, alongside other preclinical tools, to gain deeper, actionable insights into a drug – and earlier in its development. Importantly, the additional information generated enables improved planning of subsequent in vivo animal or human studies, which can ultimately save many resources.
OOC technology is customizable and advancing rapidly, but each model can only contain as much as you put into it. But that’s not to say that complex OOC models do not exist; there are some that allow a user to mimic blood perfusion and immune responses in a number of disease areas. For example, during the COVID-19 pandemic, the MPSCoRe consortium was formed to use OOC models to screen potential drugs to treat the disease. Following the pandemic, these models are now being incorporated into future pandemic preparedness programs.
OOC technology has also been developed to model inflammatory bowel syndrome and even diabetes. On the oncology side, OOC has been employed to model various tumor types, alongside critical aspects of tumor progression, such as angiogenesis and metastases. Another area in which OOC has been successful is metabolic disease, where it has even been possible to develop advanced liver models that mimic non-alcoholic steatohepatitis (NASH) – an increasingly prominent fatty liver disease for which there is no known cure.
It’s very easy for me to list the advantages here, but there are also areas in which OOC has struggled to take hold. It is particularly difficult to model neurodegeneration because of a lack of reliably available cellular material and an inability to fully differentiate and age neuronal cell cultures. OOC models need to be developed using consistent, high-quality cells to ensure data is robust and accurate – and it is difficult to procure aged human neuronal cells of a high enough quality to develop these models.
One final perceived barrier to OOC adoption is the regulatory landscape. However, my company has a long-standing collaboration with the FDA, which has helped to ensure that OOC-generated data is suitable for regulatory submissions. As a consequence, we are starting to see a shift in regulatory systems, with increasing mentions of OOC as an accepted technique. The collaboration represents active participation in the development of standard validation qualification frameworks to support ongoing efforts to standardize OOC data. Collaborations such as this, as well as participation in supportive consortia (including IQ-MPS) are beginning to showcase OOC – and how it can be used in workflows.
Overall, OOC models are poised to become a broadly accepted tool in the preclinical toolbox. They could enable enhanced prediction of human tissue responses to therapeutics and the development of a more efficient and cost-effective drug discovery process.
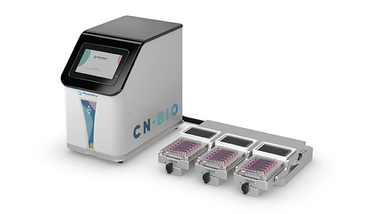
Chief Scientific Officer, CN Bio, Cambridge, UK



















