Digging into the Dangers
Research sheds new light on cancer risk in gene therapies
Jamie Irvine | | 5 min read | Interview
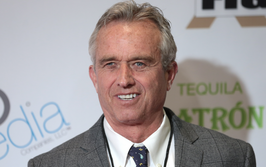
Credit: Author supplied
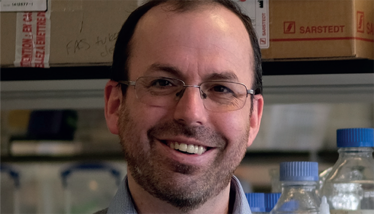
Scientists from the University of York, Boston Children’s Hospital, and the Wellcome Sanger Institute are collaborating to understand blood cancer risk in gene therapies. With funding from the Bill and Melinda Gates Foundation, the team discovered that the gene therapy process can cause blood cells to “compete” against one another with some potential risks for patients (1).
We spoke to David Kent, Deputy Head of the Department in Biology at the University of York, UK, to learn more.
What does “cell competition” involve – and what causes it to occur?
Cell competition is something that we are very familiar with in the stem cell field – we estimated in 2018 that an average adult human has around 100,000 functionally active blood stem cells. These stem cells compete against one another throughout life with old age often evidencing the “winners” of this competition via something called age-related clonal hematopoiesis or, in some cases, the development of blood cancers from single stem cells.
At its core, cell competition involves those blood stem cells undergoing stem cell expansion divisions (for example, one stem cell creating two equally potent daughter stem cells) more frequently than other stem cells, thereby acquiring a relative growth advantage and “over-contributing” their fair share of cells to the blood system. This is totally normal, but when pushed to the extreme, it can result in fewer stem cells being able to contribute (because of the complete loss of some stem cells). It is thought to occur from a combination of random chance and imposed selective pressures; for example, genetic mutations or external modifiers, such as aging bone marrow.
Can you elaborate on the specific genetic mutations observed in your study and how that relates to gene therapy?
In normal aging, a number of mutations have been described to preferentially accumulate – we think of these mutations as conferring a “resilience” on these cells that allows them to preferentially survive stressful events. The result of such mutations is relatively common in old age (clonal hematopoiesis), but in a small minority of cases, mutations in these same genes are also observed in blood cancers. Dnmt3a and Ezh2 (as described in our current paper) are two such mutations. The presence of these mutations does not mean that the gene therapy patients will develop blood cancers, just simply that cells with these mutations are not selected against during the gene therapy process.
When patients have blood cells removed for gene editing, the blood cells that are not removed are hit with drugs to destroy them, which is followed by giving these patients their own blood cells (now gene modified) back in a transplantation. I like to explain this with an analogy: if you clear a forest and then scatter some seeds back onto the ground, some seeds will grow better than others for a whole variety of reasons – with many never growing anything at all. Of the ones that survive, they will produce different numbers of progeny that may also have an advantage in growing and this results in the “competition” that occurs whereby the original handful of seeds that you scatter are no longer fairly represented in the forest. If we can understand why some “seeds” are better or worse at growing and how likely (or not) they are to lead to a blood cancer, we will be able to in turn understand how to selectively retain the less dangerous blood cells when patients undergo gene therapy.
What are the next steps for this research?
The next phase of our work will bring in new partners in Tanzania and Uganda to understand the prevalence of these mutations in large cohorts of patients in regions where sickle cell disease is far more common.
Finally, what first triggered your own personal interest in gene therapy and cancer?
It was a case of key events aligning with key moments in my training. The first was the isolation of human embryonic stem cells in my final year of high school, and the second was the completion of the human genome in my final year of undergraduate study. You can’t predict what discoveries you emerge at decision-making junctures in your life, but, for me, gene therapy and stem cell biology were at the right place at the right time and became the path I followed.
When I began my PhD journey at the Terry Fox Lab in Vancouver, I was introduced to the Keith Humphries’ research group, who had just released a huge paper detailing the use of Hoxb4 to expand blood stem cells outside the body. This marked my first exposure to the power of using genetic modification to alter cell outcomes. However, the initial excitement was tempered by reports of challenges in the first gene therapy trials involving patients’ blood stem cells. This prompted a collective pause in the field as efforts were directed towards refining the technologies involved.
During this period of advancement, my personal involvement in gene therapy took a backseat for more than a decade. And though I consistently kept up with the latest literature, my focus shifted towards the expansion of stem cells and understanding the cancers that can arise from their subversion. This most recent study and the partnerships that we have forged with Boston Children’s Hospital and the Wellcome Sanger Institute have brought me full circle, applying our decades long understanding of stem cell biology to some of the big questions in gene therapy.
- MS Chapman, et al., “Clonal selection of hematopoietic stem cells after gene therapy for sickle cell disease,” Nature (2023). Available at: doi.org/10.1038/s41591-023-02636-6
Associate Editor, The Medicine Maker