Malaysia in the Middle: Tackling Hep C in an Unfair World
How the Drugs for Neglected Diseases Initiative worked successfully with local and global partners to improve left-behind lives in Southeast Asia
When it comes to beating infectious disease, middle-income nations face a two-pronged problem: they’re too poor to pay for patented medicines upfront, and too wealthy to qualify for voluntary licenses – the charitable exceptions to patent paywalls which (in theory) improve drug access in the world’s poorest countries.
Malaysia is not one of the world’s poorest countries. In the UN’s human development index, it places at 62 out of 189 countries (1). World Bank figures from 2020 place Malaysia at 58 out of 199 in GDP per capita (2). Though Malaysia’s economy is on track to transition from “middle income” to “high income” by 2024, growth has been lopsided and the outlook is less than certain. The poorest 40 percent of the population are financially vulnerable, and more than one in 20 households lives in absolute poverty (3). Much of the population is susceptible to ailments that citizens of the world’s wealthiest countries are by-and-large shielded from – hepatitis C being a prime example. At present, around 400,000 people among Malaysia’s population of 32 million are infected.
A real burden
When asked which groups in Malaysia suffer most from hep C, Radzi Hassan, a practicing consultant physician and gastroenterologist, and recent appointee as the Head of Service for Internal Medicine under Malaysia’s Ministry of Health, says, “Based on my observation, people who inject drugs constitute the vast majority of hepatitis C patients in Malaysia. The other key populations of hepatitis C include people living with HIV, people living in prisons and rehabilitation centres, men who have sex with men, and sex workers. Generally, hepatitis C patients in the country are made up of vulnerable groups, characterized by a relatively low socioeconomic status.”
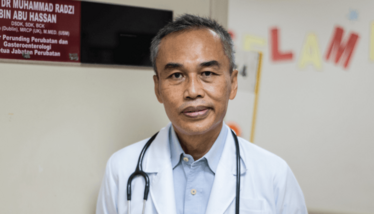
Radzi Hassan, standing in the doorway to his office.
Hassan also lays out the economic angle: “Malaysia is pursuing the global goal set by the WHO to eliminate hepatitis C as a public health threat by the year 2030; ensuring accessibility of effective direct-acting antivirals (DAAs) is exceptionally important. However, the use of DAAs in Malaysia was once restricted by their exorbitant prices. Many patients were, therefore, not treated timely and died from the chronic complications of hepatitis C, including cirrhosis and hepatocellular carcinoma. Having more treatment options can create a more competitive market for DAAs, and indirectly make them more affordable.”
In 2016, the Malaysian government introduced a three point strategy to help achieve the 2030 goal: i) seek out hep C infected patients in the country; ii) lower the price of DAAs; and iii) decentralize hep C treatment to make it easier for patients to access.
The government began working on plans to identify patients and decentralize treatment, but to achieve the pricing objective the government had to negotiate with Gilead Sciences with regards to the hep C blockbuster drug Sovaldi (sofosbuvir). The drug came with a cost of around $1000 per pill at the time - working out at around $84,000 per treatment course. The negotiations ultimately failed, but in response Malaysia issued a “government use” compulsory license, granting access to generic sofosbuvir (priced at $300). In counter-response, Gilead granted voluntary licenses to not only Malaysia but also Thailand, and Ukraine, where clinical trials of a new DAA called ravidasvir were planned.
Enter the DNDi
The Drugs for Neglected Diseases initiative (DNDi) was well aware of the price controversies surrounding sofosbuvir. The initiative was founded in 2003 after Médecins Sans Frontières (MSF) dedicated a portion of their 1999 Nobel Peace Prize to exploring a new, alternative, not-for-profit model for developing drugs for neglected patients. According to François Bompart, Chair of the Access Committee and Former Director of HIV & Hepatitis C Initiative at the DNDi, hep C treatment before sofosbuvir was complex, badly tolerated by patients, and ineffective. “Sofosbuvir brought about a total revolution: this was the first drug that could, after 3–6 months of a well-tolerated oral treatment, actually cure patients entirely and prevent people from transmitting the virus to others. This huge innovation was hailed as a ‘miracle drug.’ The problem is that this innovation was priced at a level that was unheard of at the time. Even for high-income countries, such a price level represented a major challenge. Some were able to negotiate more reasonable prices for sofosbuvir and its successors, but the drug remained out of reach for many countries.”
Shing Chang, DNDi R&D director at the time, set about looking for alternative DAA candidates. “A few years earlier, MSF had been a leading force in the global movement that fought against the high price of antiretroviral medicines (ARV) for the treatment of HIV/AIDS in Africa,” says Bompart. “DNDi and MSF therefore decided to join forces to develop a new DAA combination. The purpose of that development was to demonstrate that another way of developing new drugs was possible, led by the objective of optimizing the new drug’s public health impact, not its financial benefits, and relying on partners from the most affected countries; in other words, middle-income countries.”
In 2016, DNDi identified ravidasvir – a DAA candidate developed by the US company Presidio Pharmaceuticals that had reached phase II clinical trials – as the best possible candidate to use with sofosbuvir as a companion drug. “The treatment of HCV infection is based on a combination of drugs that act on different viral targets,” says Bompart. “It is necessary to combine drugs from different families that act on different parts of the virus’ metabolism. This increases the likelihood of an effective treatment and prevents the development of resistance. Non-structural proteins 5A and 5B (NS5A and NS5B) play a key role in hepatitis C virus RNA replication. Ravidasvir is an NS5A inhibitor and sofosbuvir in an NS5B inhibitor.”
MSF decided to fund DNDi’s development program through its Transformational Investment Capacity (TIC) initiative. One key industry partner in the project was Egypt-based company Pharco Pharmaceuticals, which had previously taken part in Egypt’s national strategy to fight hep C and shown in early clinical trials that the ravidasvir/sofosbuvir combination was highly effective in genotype 4-infected patients, the most frequent genotype found in Egypt. “Pharco’s CEO, Sherine Helmy, had expressed very early on his personal commitment to help fight HCV around the world, not as a business-based strategy, but as a public health priority. The $300–500 target price of ravidasvir at launch, set right from the beginning of the drug’s development, was a clear sign of this commitment,” says Bompart.
The DNDi has had an office in Malaysia since 2004. DNDi and the Malaysian state’s collaboration on a new hep C treatment was aided in particular by Noor Hisyam Abdullah, Director-General of Malaysia’s Ministry of Health, who holds a seat on the board of DNDi thanks to the Malaysian MoH’s historical role as one of the founding members of DNDi.
In 2016, DNDi initiated a phase II/III study in Malaysia and Thailand that aimed to assess efficacy, safety, tolerability, pharmacokinetics, and acceptability of 12- and 24-week regimens of the ravidasvir and sofosbuvir combination. The study, named STORM-C-1, was a huge success. Results published in The Lancet in April 2021 (4) showed cure rates of 97 percent, and high tolerance across a diverse adult population. The drug combination was able to cure people infected with genotype 3 of the virus, a particularly hard-to-treat variant. The study was a key cornerstone of the registration dossier that led to ravidasvir’s conditional registration by Malaysia’s National Pharmaceutical Regulatory Agency in June 2021.
If I may be provocative...
Both Hassan and Bompart agree that development has had its ups and downs. Patient enrolment was a particular concern early on because many hep C patients were reluctant to come forward. Hassan says, “We noticed that many more patients were – and still are – hiding themselves in the community, partly due to the stigmatization of the disease.” To help find participants, the government enlisted the support of the Malaysian AIDS Council, the Third World Network, and several local civic organizations, but Hassan expects that finding the “missing millions” will remain a major challenge.
Bompart adds that it’s important to remember that ravidasvir is still a very young drug. “Quite a lot of work is still needed to properly assess its key efficacy and safety features, in particular against HCV genotypes that were not tested in Malaysia and Thailand, and to find its space in the global DAA armamentarium.”
So far, however, the results of the project have been a huge success. “Malaysia is deeply honored to present a wonderful gift to the world, a new pan-genotypic and yet highly affordable DAA combination,” says Hassan. “This marks a historic moment for Malaysia as a middle-high-income country to make significant contributions in drug development for a global endemic.”
Beyond the Southeast Asian nation’s borders, Bompart hopes that the project has sent a message. “We are pursuing registration opportunities in middle-income countries where generic sofosbuvir is available or stands a high chance of becoming available. The registration file approved by Malaysia’s NPRA is our key asset. Even though this project concerned ravidasvir, we are actually advocating for access to all affordable, safe and effective DAAs that countries may choose. We are now rolling out plans to help a handful of countries improve access to all DAAs through policy, financing, and intellectual property. This is being prepared in partnership with MSF, FIND (the global alliance for diagnostics) and the Treatment Action Group.”
This recently announced partnership has been titled The Hepatitis C Partnership for Control and Treatment, or Hepatitis C PACT for short. In its mission to tackle ongoing disparities in access to diagnostics and treatment for Hep C, the “pact” will look to low and middle income countries, where three in four of all people suffering from the disease live today.
This is not simply a story of aspirations and improvements; there is a huge political dimension to the story about ensuring that all countries – regardless of economic conditions – have access to affordable therapeutics. Bompart spells it out:
“If I may be provocative: ravidasvir was developed at a time when few DAAs were available, and one can always hope to bring new benefits with a new drug. However, our agenda was largely political from the beginning, with the objective of opening the eyes of decision makers to two sets of issues: first, the realities of HCV; second, the ability that political decision-makers have to act when the abusive use of intellectual property leads to unaffordable prices that prevent access to life-saving drugs. Everywhere in the world, in rich and poor countries alike, affordable DAA prices only exist where governments fight for them.”

Sharol, a self-employed rice farmer from Kedah, who received his diagnosis of hepatitis C over 10 years ago, but chose not to seek treatment due to fear.
Following a recommendation from his doctor, Sharol registered himself for treatment. To his surprise, within 3 months, he was cured of hepatitis C with minimal side effects – a stark contrast to his fears, which had been based on his friends’ past treatment experiences.
- United Nations Development Program, “Latest Human Development Index Ranking” (2020). Available at: https://bit.ly/3iGrJFw
- World Bank, “GDP per capita (current US$)” (2020). Available at: https://bit.ly/2VOQZ3f
- World Bank, “The World Bank in Malaysia” (2021). Available at: https://bit.ly/3CFT1nq
- The Lancet, “Efficacy and safety of ravidasvir plus sofosbuvir in patients with chronic hepatitis C infection without cirrhosis or with compensated cirrhosis (STORM-C-1): interim analysis of a two-stage, open-label, multicentre, single arm, phase 2/3 trial” (2021). DOI: 10.1016/S2468-1253(21)00031-5
Between studying for my English undergrad and Publishing master's degrees I was out in Shanghai, teaching, learning, and getting extremely lost. Now I'm expanding my mind down a rather different rabbit hole: the pharmaceutical industry. Outside of this job I read mountains of fiction and philosophy, and I must say, it's very hard to tell who's sharper: the literati, or the medicine makers.