Getting Creative with Rare Diseases
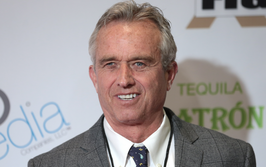
Gene Sullivan, Chief Product Strategy Officer at Insmed, explores how new thinking could improve the research process for rare disease treatments
What piqued your interest in rare disease treatments?
I was initially drawn to rare diseases – particularly rare pulmonary diseases – during my fellowship training in pulmonary and critical care medicine. I found the histopathologies and radiographic appearances fascinating, and I enjoyed the challenge of the differential diagnosis that they represented. There were very few evidence-based treatments available, leaving room for medical judgment based on current understandings of the pathobiology.
I found the challenges invigorating – they offered a less explored area with more room to continue to learn, as well as more of a challenge in making the correct diagnosis and determining the best treatment. That was my entrée into this area of medicine and science. During my time in clinical academic medicine, I focused on rare pulmonary diseases before acquiring a position at the FDA, where I reviewed drugs intended to treat interstitial lung diseases and other rare pulmonary diseases. After that, I branched out into the drug development industry.
What’s exciting right now at Insmed is our ability to move beyond a pulmonary focus into other rare and serious diseases with unmet needs. Being part of that growth is personally enriching for me because I get to learn about other diseases. It also opens room for more creativity. For instance, as we’re learning more about gene therapy, there are things we can bring from our previous research – a cross-fertilization of knowledge and ideas that is not only interesting but could also ultimately benefit patients.
What challenges are faced by patients with rare diseases?
The first challenge faced by patients with rare diseases is obtaining a correct diagnosis. Universally with rare diseases, even with the best healthcare, getting an accurate diagnosis is often delayed – we hear from patients that it might have taken them five years and many different doctors to get the right answer. Moreover, if you have poor access to healthcare and face other types of non-clinical barriers, the path to a correct diagnosis is going to be even more challenging. In the absence of a correct diagnosis, patients may endure significant unexplained symptoms and cycle through multiple misdiagnoses and associated failed attempts at treatment, which can be a very stressful, scary and isolating experience.
The next challenge that these patients often face is finding an expert to treat their disease. Primary care doctors and even local specialty physicians may have very little experience with the disease, meaning that patients may have to travel long distances to find the best care. This is not always a viable option for many patients, who do not have the necessary resources for such care.
For many rare diseases, the challenge is that there are no established treatments. In some cases, where there is sufficient understanding of the pathophysiology of the disease, doctors may be able to try to apply existing drugs in off-label fashion, but they have very little reliable data on efficacy or safety to guide them in this. And in many cases, the only option is to try to treat symptoms with non-specific interventions that don’t address the primary cause of the disease.
This last challenge is what we are keenly focused on here at Insmed, where we are working to develop drugs to treat serious, rare diseases — particularly those for which there are no current treatment options.
What’s the current landscape of rare disease research?
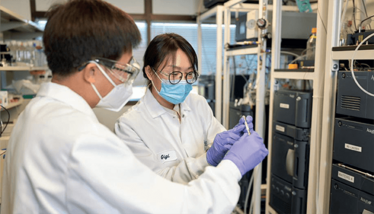
To provide some context, there are more than 7,000 known rare diseases and approximately 95 percent of them have no treatment (1); in other words, the breadth of what we classify as “rare” is vast. In the past, too little attention was paid to development of drugs to treat rare diseases; however, more recently, we’ve seen a huge uptick in interest in studying rare diseases, which has been great for the rare disease community. In the field of gene therapy, for instance, advances in our understanding of the genetics of rare diseases, combined with the development of new technologies to deliver gene therapies efficiently and safely, have allowed us to explore the field of rare monogenic disorders more broadly, opening a world of possibility for new treatments of these types of diseases.
At Insmed, we’re studying a number of rare and serious diseases, including nontuberculous mycobacterial (NTM) lung disease, bronchiectasis, forms of pulmonary hypertension, and cystic fibrosis. In addition, we have early-stage programs in gene therapies for various rare genetic disorders. Clearly, those are just a few out of the thousands of rare diseases that still have significant unmet needs.
How do you deal with the pressure of such challenging diseases?
I don’t really see it as pressure. I tend to see the various challenges associated with rare diseases more as opportunities to be creative, which is why studying rare diseases can be so interesting and fulfilling. It invites the search for novel approaches, which is liberating and exciting because there isn’t a well-trodden path. That said, one potential challenge in this field is balancing “outside-the-box” thinking with scientific and regulatory requirements. I often find myself trying to merge those two worlds – the creative approaches needed to address rare disease research and the requirement for regulatory rigor. You have to find a way to be creative within the requisite scientific and regulatory framework. After all, the goal is to generate convincing evidence to establish the efficacy of a new drug to support regulatory approval.
How can we make early stage research more effective – and what could we do better?
In all forms of clinical research, not just those for rare diseases, we need to be sure that we remain cognizant of the sacrifices and risks that trial participants take on when they agree to clinical studies, particularly studies involving investigational drugs. We always need to show deference and respect in that regard. We have an obligation to be sure that our studies are scientifically sound and that they are designed in such a way that the conclusions we draw will advance our scientific knowledge, all the while taking care to minimize the risks that subjects face as they help us learn those lessons.
Even more so in rare disease clinical research, we need to make the most of every patient’s contribution – simply because there are fewer patients from whom we can learn. If we can answer more than one question with a study, we should. And when you factor in the urgency of the need – many rare diseases are serious and without existing therapies – it becomes even more imperative that we design programs that ask and answer the right questions efficiently. Sometimes the conclusion may not always be that a new compound is in fact safe and effective. In such cases, we owe it to the patients to arrive at that conclusion as efficiently as possible so that other approaches can be studied.
Improvements could include adaptive trial designs, where emerging knowledge can be more rapidly and seamlessly incorporated into ongoing studies (rather than conducting serial, distinct trials to get where we want to go in a methodical, stepwise fashion – the traditional approach).
The actual selection of the clinical endpoint can also contribute to the efficiency of the trial. In taking the time in advance to understand the disease pathophysiology and its clinical manifestations, you may see that there is more than one aspect of a disease that may be beneficially impacted by a drug. If that is the case, we should carefully consider our selection of the primary efficacy endpoint. It may often be appropriate to focus on a particular potential clinical benefit that can be captured by a primary endpoint, which could establish efficacy with the fewest number of participants in the shortest period of time.
What are the potential downsides of such approaches?
One perceived concern is that shortcuts in clinical development might ultimately cause us to reach incorrect conclusions about a drug’s promise. Patients with rare diseases deserve drugs with a favorable risk/benefit profile every bit as much as patients with more common diseases. New, more efficient approaches should never supersede the need to rigorously evaluate both the efficacy and safety of new drugs; the conclusions we reach on those aspects must be scientifically sound. I believe there are means by which we can improve the efficiency of drug development and still preserve the integrity of the process.
Does the recruitment process also require a different approach?
Recruiting for rare disease research is more challenging so most researchers collaborate with patient organizations – many of which recognize the unique service they can offer in supporting clinical research as a means of fulfilling their mission to support patients; indeed, many have built databases of patients that can be accessed to speed up enrollment.
The other approach researchers often take – as we’ve done at Insmed when studying NTM lung disease – is engaging with centers of excellence and the experts who know the disease best. These people invariably have the most knowledge about and access to the patients we’re seeking to enroll.
With rare diseases, we know that obtaining an accurate diagnosis can often be delayed. If we can find ways to raise disease awareness and get these patients diagnosed earlier, we may find that they are candidates for clinical trials – perhaps even at an earlier stage of the disease, when therapies may be more likely to have a positive impact. In addition, taking steps to support clinical trial enrollment for all eligible patients, such as offering trials in more accessible regional centers, could improve our ability to enroll more patients more efficiently and ensure that our clinical trial populations are as representative of the overall patient populations as possible.
What are your hopes for the near future?
My hope is that we can continue to think of and explore creative ways to establish the evidence we need more definitively and efficiently while maintaining the integrity of the process. I would also like to imagine that this concept of adaptive trial designs continues to flourish by providing inferences that are statistically sound but more efficient than traditional, serialized trials.
My other hope is that we, as researchers, in the drug development industry continue to consult early and often with regulatory bodies. Regulatory bodies may be able to provide important input and guidance on challenging topics based on their prior experience of the successes and failures of development programs facing similar challenges. Pharmaceutical companies and regulatory agencies share a desire to bring safe and effective drugs to patients in need as rapidly as possible, and both have deep knowledge and relevant experience. Rich interaction and collaboration between the two will help ensure that development programs advance in the right direction, generating data that meets the needs of all stakeholders.
- Rare Disease Day, “Frequently Asked Questions” (2019). Available at: https://bit.ly/3XQv8UX
Following a Bachelor’s degree in English Literature and a Master’s in Creative Writing, I entered the world of publishing as a proofreader, working my way up to editor. The career so far has taken me to some amazing places, and I’m excited to see where I can go with Texere and The Medicine Maker.