Crafting a Magic Bullet
The field of antibody drug conjugates has seen many ups and downs, but, with new science shedding light on how to better design and engineer these therapies, it’s certainly never boring. Colin McKee, Head of Technical Services at Sterling Pharma Solutions, gets us up to speed on advances shaping this dynamic space.

Why has the concept of “magic bullets” caused so much excitement in the pharma industry over the years?
The concept of developing drugs that specifically target disease, whilst leaving healthy tissues and organs unharmed, is a key goal for the industry. The term “magic bullet” – coined by Paul Erlich in 1900 – really captures this. Antibody-drug conjugates (ADCs) are an embodiment of this concept because they are both highly effective and highly targeted. There have been several setbacks over the years, but over the last decade there have also been success stories. As one example, consider Roche’s Kadcyla, the ADC of the breast cancer antibody Herceptin by Genentech. The ADC concept was used to improve Herceptin and offer better outcomes for patients (1).
ADCs have also shown remarkable benefits against cancers previously considered hard to treat – or where traditional chemotherapies cannot achieve durable results following treatment. As an example, consider Adcetris; in patients with classical Hodgkin lymphoma after failure of auto-HSCT or after failure of at least two prior multi-agent chemotherapy regimens, and in patients who are not auto-HSCT candidates, all of whom show progressive disease, Adcetris has been shown to achieved long and durable disease control (2).
Because of these successes, and the knowledge gained in developing these molecules, the scientific community is starting to “blue sky brainstorm” and is coming up with many different ways in which these ADCs can be exploited.
What have been the highs of ADCs?
The recent approval of Zynlonta for ADC Therapeutics was an especially high point for us. Sterling (formerly ADC Bio) developed the conjugation process and performed process characterization to support the Biologics License Application (BLA). This work was carried out between 2014 and 2020, and demonstrated how quickly ADC molecules can progress from research and development to commercialization.
There is now an increasing number of ADCs gaining approval and entering the clinic each year. The value of recent deals for ADCs is also staggering; AstraZeneca and Daiichi signed a $1-billion deal in 2020 – and AstraZeneca has also committed $6 billion to Daiichi’s ADC Enhertu. Also in 2020, Merck Sharp & Dohme acquired VelosBio in a deal worth $2.8 billion (VelosBio’s lead investigational candidate is an ADC).
And what about the lows? What setbacks has the field encountered?
There are still ADCs that enter the clinic and fail to achieve the results needed to progress, which results in projects being terminated. There is still a relatively low success rate for advancing a molecule through the clinical phase to commercialization. In 2018/2019 there were some high-profile withdrawals, and a high percentage of clinical trials were terminated. But, according to one review from The Beacon database, only a handful have been terminated since then (3).
What are the biggest scientific challenges associated with designing and developing ADCs?
ADCs have many moving parts and “designing” the right combination to work against each unique disease (type of cancer) remains the biggest challenge. Finding and validating good targets is the first challenge. There are a number of well-agreed rules on which properties constitute a good target; for example, being present only on diseased cells rather than on healthy cells; internalizing the ADC; and not shedding into circulation. Many “low hanging fruit” targets have also already been addressed. For example, numerous companies have ADCs in development against HER2. Identifying new targets brings us back to the fundamentals of biology – and, as with all biopharmaceutical drugs, these are hard yards.
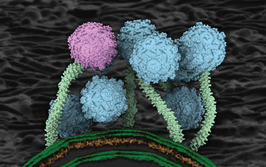
Once there is a validated target and an ADC format has been decided upon, the “fun” really begins. Making the antibody and selecting a conjugation chemistry and drug combination was once (relatively) simple, but now an ADC developer has many choices for all three main components of an ADC. Should it use a simple human mAb, or an engineered format designed for a specific conjugation chemistry? Should it focus on improving targeting to a specific cell; such as a bispecific mAb for example. Or should the ADC be engineered to stay in the cell once internalized to improve the amount of drug delivered?
Then, there are many new ways in which the conjugation can be performed, and choices to make with regards to the drug to add. It is easy to design and make ADCs that can kill target cells in test tubes and “cure” mice, but it is still a struggle to translate this science to safe and effective molecules that work in humans. An ADC team must be truly multi-disciplined: combining experts from chemistry, protein sciences, toxicology, biology, safety, manufacturing sciences, and many other fields.
Bigger pharma companies are able to build large teams of people and dedicate a great deal of resources to developing ADCs. Many different molecules can be made, tested, and optimized through iterations before being progressed and (potentially) terminated before a good one gets to market. Smaller biotechs however, may take a different approach and rely on precedent from approved ADCs, looking to quickly combine the best available knowledge and design into their specific ADC. Velos Bio, for example, moved very quickly based on a good target, ROR1, and an already available mAb, UC961, and simply followed the pathway from the development of Adcetris, using the same conjugation chemistry and toxin linker. Leveraging the vast safety data set that exists now for Adcetris allowed its ADC to get into the clinic quickly, and generate the data that really mattered – the efficacy profile in real patients. And its subsequent acquisition by Merck validates the approach!
What are the challenges associated with manufacturing?
Making either a small molecule or a protein therapeutic is already a complex process. However, when both approaches are combined into one molecule and the issues associated with the very potent nature of these molecules are taken into account, the degree of complexity further increases. The small molecule and antibody will be managed by scientists who may be used to making these as stand-alone molecules, but now they need to consider their products as raw materials for the conjugation, and understand what changes can be made without impacting subsequent steps. In addition, the regulatory and analytical requirements are a hybrid of the two very different small molecule and biomolecule disciplines. Analytics in particular are very complex, as many ADCs are a mixture of many subtly different forms of the drug, each of which needs to be understood.
The next step is to make the necessary components and combine them. This can either be done by building out that capability in-house or by outsourcing; however, there are very few experienced ADC CDMOs, and choosing one that can align with the capacity and lead times needed for a program can be challenging. Typically, it is the chemistry CMOs that work with highly potent molecules and are experts in the containment required for ADCs, but their knowledge is usually very limited in terms of biologics manufacturing. Conversely, biologics CMOs typically understand proteins and cleanrooms, but know less about the containment and the chemistries involved in making an ADC.
Why are things starting to change? What new science and approaches are emerging that could boost the ADC field?
Knowledge and understanding of ADCs is the key driver. The more we know, the better our designs will be, and the more likely we are to design out issues that have stopped other ADCs from progressing!
What activity are you seeing now in the ADC space?
ADC clients range from single academics all the way through to large pharma companies and this demonstrates the volume of work and interest in this drug format. I would say that the percentage of non-traditional ADCs we are asked to work on has been a significant change; the number of these types of projects is increasing compared with “traditional” ADCs (considered to be an antibody combined with a highly toxic small molecule drug, which directly kills the cell for use in oncology).
We are now seeing different carriers used in place of the antibody, such as peptides, nanoparticles, antibody fragments, and antibody-like proteins. The drugs are not all direct cell killing, with some now stimulating the immune system, and others amplifying the body’s natural killing mechanisms against cancer. These new ADCs have shown the ability to not only kill off a cancer, but also to provide a patient’s immune system with some memory that prevents re-growth of new cancers (4). We are also seeing the “magic bullet” concept being turned against other diseases such as infection, inflammation, and autoimmune disorders.
Now that the pyrrolobenzodiazepine (PBD) dimer payload has been truly clinically validated following the Zynlonta approval, this opens up more opportunities in that space. The termination of Abbvie’s Rova-T ADC in 2019 caused many to think that this payload class was just too toxic. However, the ADC Therapeutics success shows that the payload is manageable – as with all other highly potent ADC payloads – when combined with the correct antibody, directed to the right target, and administered in an optimized way.
What do you know about the current pipeline of ADC therapeutics?
Since the approval of Zynlonta – an ADC that we were involved with – there has been another approval. AIDEXI was approved in China in April 2021. However, we’re also working on a number of other ADC products.
It is estimated that 14 new INDs will be filed for ADCs this year, and over 100 clinical trials initiated (3). It is hard to keep apace with this field, but thankfully there are several good resources including the Beacon Database, ADC specific conferences, webinars and review publications that help by providing regular update summaries. Those in the know anticipate approvals from Seagen and Immunogen with their own and partnered ADCs. ADC Therapeutics’ next molecule, ADCT-301, is also at phase II.
Most of the ADCs close to approval use toxins that are already approved, such as auristatins, maytansines, and PBDs, but one interesting molecule is Byondis’ duocarmycin-containing ADC. Duocarmycins were used in some early ADCs by BMS/Medarex without much success, so seeing a promising one in the clinic is good for that payload class.
Despite the setbacks, why do you remain excited by the future of ADCs?
I make ADCs and I like the challenges that this work brings. It is clear that these molecules are at the very least transformative, and maybe one day we will use the descriptor “curative” for them. Helping ADC developers get new molecules into the clinic and to the patients who need them excites me. In doing so, I learn something new every day – be it a new analytical technique to answer a question we could not answer previously or a new conjugation method that overcomes challenges. There is a lot of innovation in this field – and it is never boring.
- CE Geyer Jr et al., “Phase III study of trastuzumab emtansine (T-DM1) vs trastuzumab as adjuvant therapy in patients with HER2-positive early breast cancer with residual invasive disease after neoadjuvant chemotherapy and HER2-targeted therapy including trastuzumab: Primary results from KATHERINE.” Presented at the 2018 San Antonio Breast Cancer Symposium; December 5, 2018. San Antonio, USA. Abstract GS1-10.
- L Gandolfi et al., “Long-Term Responders After Brentuximab Vedotin: Single-Center Experience on Relapsed and Refractory Hodgkin Lymphoma and Anaplastic Large Cell Lymphoma Patients,” Oncologist 21, 1436-1441 (2016). DOI: 10.1634/theoncologist.2016-0112
- Beacon, “ADC Beacon Targeted Therapies,” (2021). Available at: https://bit.ly/3BbJym8.
- SE Ackerman et al., “Immune-stimulating antibody conjugates elicit robust myeloid activation and durable antitumor immunity,” Nature Cancer 2, 18-33 (2021). DOI: 10.1038/s43018-020-00136-x

Making great scientific magazines isn’t just about delivering knowledge and high quality content; it’s also about packaging these in the right words to ensure that someone is truly inspired by a topic. My passion is ensuring that our authors’ expertise is presented as a seamless and enjoyable reading experience, whether in print, in digital or on social media. I’ve spent fourteen years writing and editing features for scientific and manufacturing publications, and in making this content engaging and accessible without sacrificing its scientific integrity. There is nothing better than a magazine with great content that feels great to read.