Don’t Have Your Fake, or Eat It
Finding counterfeit antibiotics – using a color-changing paper test
The fight against fake pharma continues: researchers at Colorado State have developed a simple way to detect counterfeit antibiotics using a low-cost paper test. Researcher Charles Henry tells us more.
What was the inspiration behind the test?
For the last decade, I’ve been working with other scientists in the developing world and I learned much about how healthcare works – or doesn’t work – in those countries. This piqued my interest in developing low-cost tests that could improve healthcare for people living in those areas. At the same time, Kat Boehle and I were working on a test for anti-microbial resistance. The test uses an enzyme that bacteria natively produces when it is resistant to some antibiotics to determine if the bacteria is present. In some respects, it was using the bacteria’s own machinery against it. Kat and I realized we could use that same enzyme to test for antibiotics using an assay that was both unique and low-cost (1).
How does the test work?
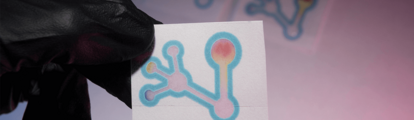
The user simply needs to dissolve the antibiotic in water and add this to the paper-based assay. It then travels down a channel in the paper containing dried nitrocefin, rehydrates the substrate, and is transported to the detection zone where betalactamase is stored. If the antibiotic is not present or diluted, the betalactamase will react with nitrocefin, causing the paper to turn from yellow to red. However, if the antibiotic is genuine, it will outcompete the nitrocefin to bind with betalactamase, resulting in no color change (remaining yellow). The pH indicator section of the paper acts as verification for whether the test is working correctly – alkaline and acidic solutions will not turn the test as red other samples. Basically, if the test does not turn red, it is a legitimate antibiotic, and if the pH indicator shows an alkaline or acidic pH, the user knows that the enzyme reaction is not working and should be cautious.
How do you envision it being used in the field?
We see the test being used primarily by individuals in the developing world. We are hoping that by making the test inexpensive and user-friendly, everyday people can take charge of identifying falsified antibiotics so that they can get the best treatment possible. Also, scientists who study falsified and substandard antibiotics around the world currently have to gather samples in the field and transport them to a central laboratory for expensive and laborious testing – so the test could save time and money. We also hope that by identifying falsified antibiotics before they are taken, less broad spectrum antibiotics will need to be prescribed, which should help slow the emergence of antimicrobial resistance.
What are your plans for the future?
First, our current test needs some additional optimization. When blind-testing different users to confirm the user-friendliness, the most commonly misinterpreted sample was differentiating between legitimate antibiotics and aspirin. This is an area we would like to address for more confident results by users. Additionally, although we have demonstrated that this assay can quantify active ingredients, a desktop scanner and image analysis program is necessary. We would like to develop a cell phone application or portable Raspberry Pi program for users who want to quantify the active ingredient – instead of the simple yes or no answer that is currently in place.
- J KE Boehle et al., “Paper-based enzyme competition assay for detecting falsified β-lactam antibiotics”, ACS Sens, 3, 1299–1307 (2018). DOI: 10.1021/acssensors.8b00163.
A former library manager and storyteller, I have wanted to write for magazines since I was six years old, when I used to make my own out of foolscap paper and sellotape and distribute them to my family. Since getting my MSc in Publishing, I’ve worked as a freelance writer and content creator for both digital and print, writing on subjects such as fashion, food, tourism, photography – and the history of Roman toilets. Now I can be found working on The Analytical Scientist, finding the ‘human angle’ to cutting-edge science stories.



















