Flu Fighters
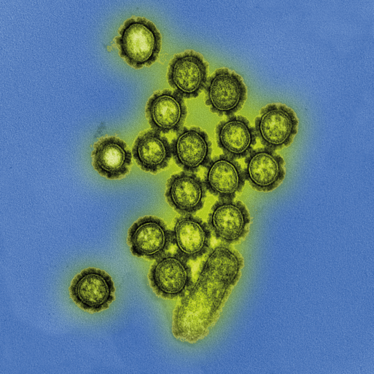
Researchers look to the ancestral genes of influenza to develop a new approach to vaccination
A truly universal flu vaccine continues to evade scientists, but it should be possible to develop a vaccine that offers broader strain protection – and lasts longer. Eric Weaver, assistant professor at the University of Nebraska, certainly believes we can do better when it comes to influenza vaccines; his team have developed a vaccine that carries the centralized genes for H1, H2, H3, and H5, with the aim of providing immunity against all evolved strains (1). We speak with Weaver to learn more.
What inspired a centralized gene approach?
I was introduced to this concept while working on HIV vaccines. Both influenza and HIV have very high degrees of diversity in the surface glycoproteins. The centralized genes act to reduce the genetic distance between the vaccine and the contemporary wildtype strains. Therefore, they offer maximal genetic identity to unknown or mismatched challenge viruses. We have published many research articles describing this approach and showed that it was a superior approach to using a wildtype immunogen as a vaccine.
How successful was your vaccine in the study?
I believe that in the context of a prime/boost viral vectored vaccine platform, our vaccine is superior to any vaccine that has been tested. The level of protection against highly divergent lethal influenza challenges is underscored in our recent study. The fact that the vaccinated mice showed no disease when challenged with 100 MLD50 of influenza virus is incredible, given this is enough virus to kill 50 mice.
Our vaccine has great potential for proving high levels of cross-protective immunity against a very wide array of divergent influenza, and the prime/boost strategy that we used could establish a foundation for immunity that will last longer than today’s vaccines.
What thoughts have you given to scale up?
We are very excited to move forward! One major caveat to this approach is that we are using a viral vector. One vector, Ad5, has been used extensively in clinical trials, but it was found that, in adults, there is a high level of pre-existing immunity that impaired the vaccine’s efficacy in preventing HIV infection. We don’t know if this will happen if the vector is used for influenza. The second vector we used, Ad4, has been given to millions of military recruits and is FDA-approved for use in vaccines. It is very likely that we could translate this vector for human use.
What other influenza projects have caught your eye?
I think there is a lot of promise in the approaches by Paleses, Krammer and Garcia-Sastre with their HA “stalk” directed immunity. The stalk domain of influenza is much more conserved than the globular head, but the immune system recognizes the head domain predominantly and therefore does not induce dominant immune responses against the stalk. These researchers are investigating novel approaches to “trick” the immune system into generating immunity against the more conserved stalk domain. If successful, this approach would certainly increase the breadth of immunity against divergent influenza strains. Perhaps a combination of this approach and our approach could lead to even better influenza vaccine results…
Some have said development of a universal flu vaccine is impossible…
It may be impossible to make a universal vaccine for everyone because people don’t respond to vaccines in the exact same way, but that argument can be made for any vaccine that has ever been used and should not be a limitation to the pursuit of new vaccine research.
- A Lingel et al., “Efficacy of an adenoviral vectored multivalent centralized influenza vaccine”, Sci Rep, 7, 14912 (2017). PMID: 29097763.



















