Nonthreatening Needles
No-one likes getting injections. Fortunately, patients may soon have a pain-free alternative in the form of microneedle delivery systems – a hot area of research for our group and others around the world.
Lifeng Kang |

So what is a microneedle? The simple answer is that it’s just like a normal needle, but on a micrometer scale. Microneedles also differ from conventional needles in that they are almost always found in an array, with several hundred tiny needles arranged in a grid. Drugs can be incorporated inside the needles or as a coat over the surface of the array.
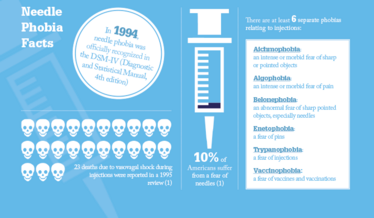
The needles are small but there are big advantages to the technology. The most obvious benefits come when we consider using microneedle arrays in place of a traditional hypodermic injection. Children are often afraid of injections, and it’s thought that more than 10 percent of adults have a needle phobia (1) – see “Needle Phobia Facts”. While we may call them needles, microneedles are almost invisible to the naked eye and painless to apply – they feel like a piece of Velcro and so shouldn’t trigger the same concerns.
Importantly, while the needles are tiny compared with standard needles, they are big enough to allow delivery of even large biologic molecules, which are in serious need of new delivery options. Even for those without a phobia, injections are typically painful and inconvenient, especially for drugs like insulin that require regular dosing. There is also the embarrassment factor of having to use injector pens or syringes in front of friends or colleagues – this is a real concern for teenagers particularly. Microneedles can be assembled into single-use, disposable patches, so it should be easy for patients to self-administer.
Other transdermal delivery mechanisms – patches, creams, gels and lotions – have been explored in the past, but the skin is a very strong barrier that most chemicals or biologics cannot penetrate. Microneedle arrays create many micro-scale passages across the outer layers of the skin, allowing the drug to enter the body in much larger quantities. It could be said that microneedles combine the best of both worlds – the effective drug delivery of injection and the pain-free, easy administration of a cream or transdermal patch.
Micromanufacturing
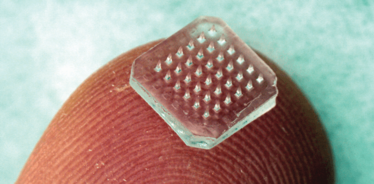
One method for producing a microneedle array is by micro-molding. Long before being applied in healthcare, micro-molding was being used in the electronic industry to manufacture computer or smart phone chips, so the technology is already well established. Microchips are usually made of silicone, but for healthcare applications we usually use metals or polymers that have an established safety profile in medical devices. Polymers used in microneedles can be designed to dissolve once inserted into the skin, releasing the drug as they do so.
My group has recently developed a new method for creating microneedle arrays using photolithography (2). The needles are made from a light-sensitive liquid, which polymerizes when exposed to light. We apply a photo-mask – essentially an opaque sheet of plastic with small transparent windows at regular intervals. Then we turn on the lights and see the microneedles form as the liquid solidifies. This simple procedure, potentially scalable for mass production, offers the possibility of conveniently incorporating the therapeutic agent inside the microneedles.
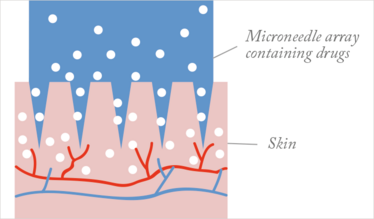
Figure 1. Microneedle patch.
Expanding applications
Given the potential advantages of microneedles, it’s no surprise that their use is being explored in a whole host of clinical and non-clinical applications. In the less regulated cosmetic market, microneedles in the form of ‘derma rollers,’ are already in widespread use. And though it’s hard to test claims that microneedles (alone or used with creams) rejuvenate the skin, we have conducted studies on topical delivery of collagen and copper peptide, which play important roles in skin regeneration and healing, but are too large to easily pass through the skin barrier. Using microneedle pretreatment increases the uptake of both molecules into the dermis significantly, with potential applications in medicine as well as cosmetics.
Another area in which microneedles show promise is in topical pain relief, and this has been a major research focus in my lab. Specifically, we have developed a microneedle patch for administration of lidocaine. Lidocaine in gel or patch form is already in common use as a topical anesthetic before injections, or to relieve local pain. However, it is relatively slow to act, taking 20–30 minutes to cross the skin and start working. If you imagine a busy vaccination clinic, that’s a significant wait between applying the patch and being able to administer the vaccine. In animal studies, we have shown that lidocaine penetrates the outer layer of skin in less than 5 minutes using microneedle patches.
Vaccination is another area in which microneedles could represent a major advance. After all, the pioneering smallpox vaccination developed by “father of immunology” Edmund Jenner was first administered by scratching the skin. Recent research indicates that if a self-administrated patch were available, significantly more people would opt for an annual flu vaccination (3). The same study found that most people were able to successfully apply a prototype patch themselves. Many groups are exploring microneedle vaccination, with promising preclinical results for flu, anthrax and others.
With multiple microscale passages created inside the skin, the delivery of various fragile biomolecules becomes possible. Microneedles, therefore, may have big potential in the world of pharmaceutical products (see “Microneedle Trials to Watch”).
.....Jeong-Woo Lee, Georgia Tech
Microneedle Trials to Watch
Eye disease (Georgia Institute of Technology)
Scientists at Georgia Tech have developed a microneedle patch for use on the eye. The patch could be used in place of eye drops for conditions like glaucoma. Eye drops, while convenient, require daily use and have poor compliance – by giving a pain-free microneedle injection in the doctor’s office, patients may be less likely to forget their medication. Hypodermic injections into the center of the eye are increasingly common, but the researchers think a microneedle patch may be more effective as it delivers the drug exactly where it needs to go.
Polio vaccination (Georgia Institute of Technology and Micron Biomedical)
Polio is one of the success stories of immunization, with cases down 99 percent since 1988. To hit 100 percent, it is essential that children continue to be vaccinated, even where the risk is very low. However, the cheap and convenient live attenuated oral vaccine carries a small risk of developing the disease, so its use is being phased out in regions where polio is no longer a threat. The problem is that the inactivated vaccine must be injected, meaning it is more expensive and must be administered by healthcare workers. Georgia Tech and Micron Biomedical recently received a grant from the Bill and Melinda Gates Foundation to develop a microneedle patch that could combine the ease of use and low cost of the oral vaccine with the safety of the injectable.
Osteoporosis (Zosano)
Eli Lilly recently bought the rights to Zosano’s ZP-PTH, one of the few microneedle delivery systems that has already undergone clinical trials. ZP-PTH delivers parathyroid hormone to stimulate new bone development in patients with osteoporosis, giving doctors and patients an alternative to injection. It was found to be safe and effective in Phase II trials, and is now moving into Phase III development.
Big future
Microneedles may even move beyond the skin, with at least one lab exploring the potential for ‘microneedle pills’ (4). Insulin was encased in an acrylic capsule covered in microneedles, with a coating that dissolves in the acidic pH of the stomach. In pigs, the pills succeeded in injecting insulin into the digestive tract lining, and did not appear to cause any tissue damage. Such advances could open up whole new fields in the microneedle area.
Drug delivery is the most obvious application of microneedles, but let’s not forget that they are still needles and could also be used to collect samples. Rather than taking a blood sample, microneedle patches could be used to painlessly collect a sample of fluid from the skin. For example, a recent study showed that biomarkers of malaria infection could be collected from mice using a wearable patch – one day this could be used to diagnose infection quickly and easily in resource-limited settings (5).
Regulatory hurdles
Microneedles are still a long way from the clinic in most cases. A few systems are now in clinical trials, like Zosano’s ZP-PTH, which delivers parathyroid hormone to osteoporosis patients. However, regulatory approval is complicated by the fact that a microneedle array is both a medical device and a drug delivery system – they have to be proved safe and effective from both perspectives. Furthermore, it is a new area for regulators as well as scientists – prior experience in regulating microneedles is lacking. There is still a lot of basic preclinical work needed to elucidate the biocompatibility of different materials and the geometry of microneedles. These factors are likely to be different for each new drug, so researchers may have to come up with a unique microneedle delivery system, compatible with that specific drug, for each medicine. Researchers will have to do more to show the nature of this new technology, but I believe once one product is approved, it will open the floodgates and we will see microneedles taking a prominent position in the drug delivery toolbox.
- J.G Hamilton, “Needle Phobia: A Neglected Diagnosis”, J Fam Pract. 41(2), 169-175 (1995).
- J. S Kochhar et al., “Direct Microneedle Array Fabrication Off A Photomask To Deliver Collagen Through Skin”, Pharm Res. 31(7), 1724-1734 (2014).
- J.J Norman et al., “Microneedle Patches: Usability And Acceptability For Self-Vaccination Against Influenza”, Vaccine 32(16), 1856–1862 (2014).
- J. Traverso et al., “Microneedles for Drug Delivery via the Gastrointestinal Tract”, J. Pharm. Sci. 104(2), 362-367 (2015).
- K. T. Lee et al., “Capture of the Circulating Plasmodium falciparum Biomarker HRP2 in a Multiplexed Format, via a Wearable Skin Patch”, Anal. Chem. 86 (20), 10474–10483 (2014).
A Lecturer at the Department of Pharmacy, National University of Singapore.



















