Big Problem, Mini Solution
Researchers have designed a “mini gene” therapy that could hold promise for treating Usher Syndrome Type 1F
Jamie Irvine | | 6 min read | Interview
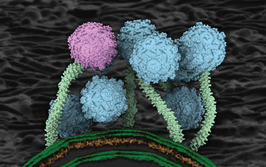
Usher Syndrome Type 1F is an inherited disease that causes profound hearing loss from birth and impairs vision from adolescence. At Harvard Medical School and the Ohio State University, researchers have developed a “mini gene” approach that they believe could help to treat the disease. Their study, published in Nature Communications, focuses on protocadherin-15 (PCDH15), a protein found in the inner ear receptor cells that, when mutated, gives rise to the unraveling of this syndrome.
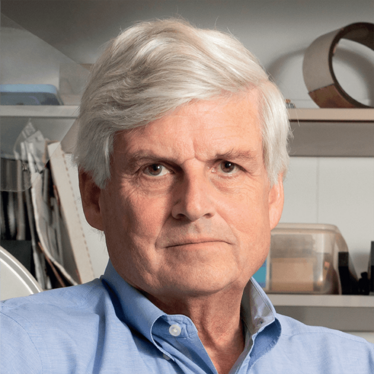
We spoke with David Corey, Professor of Neurobiology at Harvard Medical School, to learn more.
What inspired you to research Usher Syndrome type 1F?
For many years, our research efforts have focused on understanding the basic process by which the inner ear converts sound to neural signals for the brain. Though we have managed to identify a number of proteins in the inner ear receptor cells that mediate conversion, one specific protein we are particularly interested in is protocadherin-15 (PCDH15). While working on the basic biology of PCDH15, we were aware that mutations could lead to protein dysfunction, which can cause deafness and blindness: symptoms characterized by Usher syndrome type 1F.
After attending a workshop organized by the Usher 1F Collaborative with a group of patients and families, the research moved from simply trying to understand PCDH15 function to trying to develop a therapy. We were deeply moved by how devastating this disease can be for patients and the day-to-day challenges they face. Ultimately, we knew a lot about PCDH15; we felt that if we didn’t try to do something, there were few others who could.
How was the “mini gene” concept developed?
Gene therapy felt like the most obvious treatment option for Usher 1F; we wanted to get a functional version of the PCDH15 gene inside the affected cells in the inner ear and the eye. But there was a big problem – the viral vector commonly used to deliver therapeutic genes into cells is small and can only hold about 4,700 “letters” of DNA. For PCDH15, you need nearly 6,000. We knew how other labs had tried to solve this problem for other genes, and based on their research, we formulated three different strategies to solve the problem.
- We put the DNA for a “gene editor” protein into the vector, allowing the editor to find and correct the specific mutation in the receptor cells’ own DNA. This worked, but only modestly.
- We cut the DNA for PCDH15 in half, and put each half in a different vector. If the two vectors get into the same cell, some DNA tricks rejoin the DNA halves to make the full length PCDH15. This approach worked better, but still not well enough.
- We engineered a mini-PCDH15 that, despite being shorter, could still function normally. This strategy relied on the precise arrangement of atoms in PCDH15, painstakingly solved over many years by our collaborator, Marcos Sotomayor. PCDH15 has a chain-like structure, with eleven links. We knew that each end of the chain is shackled to other proteins, but realized that the links in the middle could potentially be cut out. The hardest part of this was rejoining the chain where the previous links were removed, to ensure the chain would remain strong. Altogether, we tested eight different versions to increase our chances of success.
In approach number 3, we tested the three best-performing versions in a different viral vector. We genetically engineered a mouse to have Usher syndrome 1F, and each version of the viral vector was injected into the inner ears of newborn mouse pups with the disease to see if it would prevent deafness. We then examined the inner ear to see if the normal PCDH15 protein was made; if it was located in the correct place in the receptor cells; and if it restored the normal shape of the cells. We also tested hearing after a month to see if the normal electrical signals were going to the brain. One of the mini-PCDH15 versions didn’t work at all; a second worked partially but damaged hearing in normal mice; and the third – version 4 – worked quite well. We were thrilled!
Quite frankly, we weren’t sure the mini gene strategy would work at all. Everything had to be perfect in the protein engineering to preserve the strength of the chain. The fact that only one of the eight versions could prevent deafness in the mice shows how exact the engineering had to be. We were lucky that we got one. And to be honest, science doesn’t often have “Aha” moments, where a new discovery or therapy is suddenly clear. Usually it involves some progress, then setbacks, then trying new ideas until a solution slowly emerges. But it was pretty exciting when the first mice started showing nearly perfect hearing.
Could the approach be effective in preventing blindness associated with the syndrome too?
Yes, we think so! In fact, we are rather optimistic about restoring vision in Usher 1F patients some time soon. In the Usher 1F mice, the receptor cells degenerate within a few weeks after birth, and without those cells present, there’s no place to deliver the mini genes. In humans, the cells might be gone even before birth. However the blindness in Usher 1F patients takes years to develop, so there is lots of time to deliver a mini gene to the retina. Furthermore, we believe the demands on PCDH15 in the ear are greater than the demands in the eye. We are now testing mini-PCDH15 version 4 in an animal model with Usher 1F blindness, and initial results have been encouraging.
What are the next research steps?
To move towards a clinical trial for preventing blindness in Usher 1F patients, it is essential to show that a gene therapy delivering mini-PCDH15 works in the eye, and does not damage vision. However, before testing in human patients, we must continue with the animal model of Usher 1F blindness to ensure the results are robust and reproducible. This will involve testing the therapy in non-human primates to see if the protein is functionally made, and targets the right place in the cells. Furthermore, we will also test for any toxic effects in the primates. If satisfied, we will then approach the FDA about the prospect of a clinical trial.
I should add, it has been immensely difficult to get the work funded and the results published. Even though our results are promising in rescuing hearing in mice, this is not immediately translatable to humans. While our realistic target is restoration of vision, the research did not initially address that. But some groups had faith in the long-term success of the project, and we are grateful especially to the Usher 1F Collaborative, to the Bertarelli Foundation, and to Harvard Medical School for funding our ongoing research.
Associate Editor, The Medicine Maker