The Bioavailability Toolbox
How can we overcome bioavailability challenges in our increasingly complex drug pipeline?
The Medicine Maker × Catalent Applied Drug Delivery Institute
There is no ‘one size fits all’ solution to overcoming poor solubility and bioavailability, while delivering an oral dosage form preferred by patients, as we discussed in the first article in the series (”Connecting the Dots in Drug Delivery”). Marrying acceptable solubility with long-term stability is a tough challenge that requires an array of increasingly ingenious formulations.
Since the advent of combinatorial chemistry and high-throughput screening in the 1990s, bioavailability challenges have become more and more complex. In response, new formulations and delivery methods have emerged. The result? Scientists now have an arsenal of techniques to choose from. “It used to be that micronization and the particle-forming step were all that you had, but now with the different formulation options, scientists have a much greater chance of improving bioavailability,” says David Igo, Director of Product Development and Manufacturing at Catalent Pharma Solutions.
All the patient sees is a simple tablet or capsule – only a pharmaceutical scientist knows the years of painstaking work that have gone into creating that ideal formulation.
Here, we take a whistle-stop tour of the technology and techniques that enable progress in formulation, focusing on the latest and greatest advances.

Amorphous APIs
Early in the drug development process, a process of solid-state optimization can increase the solubility of the native active pharmaceutical ingredient (API), a much less expensive option than developing complex formulations later on. The ‘go to’ method for acidic or basic compounds is to identify a suitable crystalline salt of the API, but for some of today’s candidate drugs even this option is not straightforward. “Molecules are getting progressively bigger and more complex, and this complexity means that salt formation is sometimes not sufficient to achieve a meaningful improvement in solubility,” explains Igo.
An approach that has grown rapidly in popularity over the past decade is the creation of an amorphous solid dispersion. With no crystal structure to break down, amorphous compounds are much more easily dissolved in the GI tract, exhibiting 10,000-fold increases in apparent solubility (1). Amorphous solutions are formed by combining the API with a suitable polymer, by spray drying, hot melt extrusion or co-precipitation, depending on the melting point and how easily they can be dissolved in common organic solvents.
The downside of amorphous formulations is that the physical form of the compound is generally less thermodynamically stable than a crystalline form. This can result in a shorter shelf-life due to the potential of the drug to revert to a crystalline form over time. However, recrystallization can be prevented by understanding and carefully managing the product storage condition relative to the glass-transition temperature or selection of the polymeric carrier, incorporating stabilizers into the polymer or controlling pH (2).
Super dry
Spray drying has been the most widely used method to date, with the API–polymer mix dissolved in an organic solvent, atomized and then rapidly dried with hot air or nitrogen into a fine powder. Spray drying has allowed commercialization of many drugs that would otherwise have failed, says Filipe Gaspar, Vice President of R&D at Hovione. “It is an enabling technology and we have worked on many products that only became bioavailable by adopting it and in many others that became effective drugs at much reduced dose.”
So what’s next for spray drying? There has been a lot of progress in process analytical technology, according to Gaspar, which allows continuous monitoring of critical quality attributes such as particle size or solvent content. Other areas of innovation include advanced modeling of the process, which provides for seamless scale-up and process optimization with minimum testing, optimization in the capture of the powders and more efficient operation and cleaning of the units. Considering the comparatively gentle nature of the process and recent advances in sterilization of spray dryers, Márcio Temtem (group leader, Particle Design & Pharmaceutical Development at Hovione) believes the next logical step will be to apply the technique in the manufacture of sterile biopharmaceuticals, in place of freeze-drying: “The technology has significant advantages over lyophilization in terms of cost and throughput. I would say it is just a question of time before its use becomes widespread.”
Hot topics in hot melt extrusion
Hot melt extrusion has been underutilized by the pharmaceutical industry, according to Michael Repka, Chair and Professor at The University of Mississippi. “Even though hot melt extrusion has been in use for years, many pharma companies have not fully accepted it. They have been making tablets the same way for 40 years and can be reluctant to replace older technology.”
But for APIs with the right properties, the use of hot melt extrusion is rapidly gaining popularity. As the process relies on heat and shear stress to effect molecular mixing and create an amorphous dispersion, there is no need for toxic organic solvents – or the expense and environmental hazard of removing them.
Repka’s lab experiments with a variety of different APIs, polymers, temperatures and dosage forms to find the optimum process and to troubleshoot problems, such as recrystallization or high melting point drugs. “Ultimately, our research aims to make hot melt extrusion more efficient and ideally develop platform technologies, so we don’t have to start from scratch for every new chemical entity,” says Repka.
Recently, the group was successful in using hot melt extrusion alongside high-pressure homogenization to produce solid lipid nanoparticles in a continuous process (3). Repka believes that capitalizing on the inherent continuous processing capabilities of hot melt extrusion will be crucial, as the industry (tentatively) moves towards continuous manufacturing: “If you can develop a continuous rather than batch process, that saves a tremendous amount of time and money and personnel, which means that we can get the product to the patient faster.”
“It won’t come overnight”, says Repka, “but as the equipment becomes better and better, and our understanding of the process grows, more and more pharma companies will come to accept hot melt extrusion as a mainstay.”
Size matters
For a crystalline drug, one way to increase solubility during formulation is to reduce the particle size (increasing the surface to volume ratio increases the rate of dissolution in the gastrointestinal tract). It’s now possible to reliably produce even the smallest particle sizes in either a ‘top down’ (for example, milling or micronization) or ‘bottom up’ (for example, precipitation) fashion. Micronization is the most common approach, with companies offering ever-faster and more efficient milling techniques.
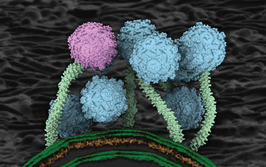
As well as increasing the surface to volume ratio, nanoparticles have intrinsic properties that can help overcome poor bioavailability. The transition from micro- to nano-scale dramatically changes the physicochemical properties of the particles, increasing saturation solubility, speed of dissolution, and the ability of the particles to adhere to cell membranes (4).
Plus, there are special advantages when it comes to targeting cancer. Ronak Savla, a Rutgers University Research Fellow supporting the Catalent Applied Drug Delivery Institute, used specially engineered nanoparticles to deliver highly potent cancer drugs specifically to the tumor site (5). “There is a phenomenon known as the enhanced permeation and retention effect in solid tumors – the blood vessels in the tumor become leaky, allowing the nanoparticles to exit the blood stream only at the tumor site rather than elsewhere in the body.”
Savla also applied cutting edge techniques to create nanoparticles for pulmonary (inhaled) delivery (6). Particle size is key for inhaled formulations, as Savla explains: “The location where the drug particles deposit is highly dependent on size, so if you want to reach the alveoli, deep in the lungs, you need a smaller particle size, whereas if you want to reach the upper airway or bronchus, you need a larger size.” It is likely to be a few years before we see the results of Savla’s work in the clinic, but experts agree that nanoparticles are a key drug delivery system for the future.
Fat chance
Lipophilic drugs are often better absorbed when taken alongside a fatty meal, a fact which gives a clue to another formulation approach for highly lipophilic compounds. Self-emulsifying drug delivery systems (SEDDS) are created by dissolving the API in a mixture of oil, surfactants and other excipients, which results in a liquid or paste intermediate that can be encased in a soft gel or hard shell capsule. After ingestion, the coating dissolves and the mixture is released into the aqueous environment of the gastrointestinal tract. The excipients added earlier cause the mixture to emulsify in the gastrointestinal tract, forming very small, easily absorbed droplets of dissolved API.
Many poorly soluble drugs also have low permeability. Lipid-based drug delivery systems enhance passive transport through the lipophilic cell membrane and tap into the body’s own mechanisms for absorbing fats through the lymphatic system.
New developments in soft gel technology have made it possible for a broad range of drugs to be developed using these techniques. Coated capsules can now delay release of the drug until the capsule reaches the lower intestine – useful for drugs that might cause gastric side effects or where efficacy would be disrupted by the acidic environment of the stomach. In addition, abuse deterrent coatings are available for products like pseudoephedrine, which can otherwise be converted by ‘kitchen chemistry’ to illegal methamphetamine.
Where a solid dosage form is preferred, solid SEDDS have been developed, using solidification techniques, such as spray drying, to convert the liquid intermediate into a standard solid oral dosage form (7).
Winning combinations
Naturally, these approaches do not operate in isolation – they are all part of the wider drug delivery toolkit, where advances in one area often trigger exciting new developments in others. For example, amorphous drug nanoparticles have shown a lot of promise, combining as they do the high solubility of the amorphous state with the rapid dissolution of nanoparticles (8). In a similar vein, the use of nanoemulsions has previously been limited by issues of palatability and formulation, but in combination with self-emulsification and soft gel technologies, nano-SEDDS are now a hot area for research (9).
Ralph Lipp, founding advisory board member of Catalent’s Applied Drug Delivery Institute, believes collaboration is key to addressing bioavailability challenges. “It is very important that there is good communication between the drug design and formulation teams within an organization. We need a team approach; a more holistic way of developing drugs,” he says.
Collaboration is central to the mission of the Catalent Applied Drug Delivery Institute, which brings academic and industrial scientists together to address current drug delivery challenges. David Igo, Michael Repka and Filipe Gaspar have all contributed to the Institute’s regular educational symposia and you can find out more about the next two events in “Collaborate and Innovate”.
Despite the range of options now available, scientists can’t rest on their laurels – they must work continuously to improve and refine current technologies – and come up with new ones. Gaspar says, “Today, the vast majority of new drugs are poorly soluble and that is a major challenge, but it also creates opportunities for new technologies to be developed in the industry.” So innovation is also essential.
In the next article in the series, we’ll be gazing into our (amorphous) crystal ball, to see what disruptive technologies will be shaking up drug delivery in the years to come.
Collaborate and Innovate
The Journey to Optimizing Outcomes: Advances in Drug Delivery & Design
March 12, 2015 Pfizer Cambridge Campus, MA, USA
- Dave Miller on solubility issues
- Stephen Tindal on lipid based drug delivery applications
- Ben Maynor on nanotechnology
- Shahar Keinan from Cloud Pharmaceuticals on data driven drug design
Addressing the Challenges of Drug Delivery: Patient Centric Design, Non-invasive Delivery of Macromolecules, Bioavailability & Solubility
April 30, 201, 3M Customer Innovation Center, Bracknell, UK
- Ralph Lipp on using patient insights to design drugs
- Mark Tomai on increasing the effectiveness of vaccines
- Claus-Michael Lehr on innovative drug delivery methods
Find out more at www.drugdeliveryinstitute.com/events
- C. Brough, and R.O. Williams 3rd, “Amorphous Solid Dispersions And Nano-Crystal Technologies For Poorly Water-Soluble Drug Delivery”, Int J Pharm. 453(1), 157-166 (2013).
- Y. Huanga and W-G Daib, “Fundamental Aspects Of Solid Dispersion Technology For Poorly Soluble Drugs”, Acta. Pharm. Sinica B 4(1), 18-25 (2014).
- H. Patil et al., “Continuous Manufacturing Of Solid Lipid Nanoparticles By Hot Melt Extrusion”, Int. J. Pharm. 471(1-2), 153-156 (2014)
- S. M. Alshahrani et al., “Stability-enhanced Hot-melt Extruded Amorphous Solid Dispersions via Combinations of Soluplus® and HPMCAS- HF”, AAPS PharmSciTech (January 2015).
- R. Savla et al., “Tumor-Targeted Responsive Nanoparticle-Based Systems For Magnetic Resonance Imaging And Therapy”, Pharm. Res. 31(12), 3487- 3502 (2014).
- R. Savla and T. Minko, “Nanotechnology Approaches For Inhalation Treatment Of Fibrosis”, J Drug Target. 21(10), 914-925 (2013).
- Tan, S. Rao and C. A. Prestidge, “Transforming Lipid-Based Oral Drug Delivery Systems Into Solid Dosage Forms: An Overview Of Solid Carriers, Physicochemical Properties, And Biopharmaceutical Performance”, Pharm. Res. 30(12), 2993-3017 (2013)
- W. S. Cheow et al., “Amorphization Strategy Affects the Stability and Supersaturation Profile of Amorphous Drug Nanoparticles“, Mol. Pharmaceutics 11(5), 1611–1620 (2014).
- A. A. Date et al., “Self-Nanoemulsifying Drug Delivery Systems: Formulation Insights, Applications And Advances”, Nanomedicine (Lond). 5(10), 1595-1616 (2010).