CRISPRing Up Brown Fat
The first steps towards an autologous cell therapy for obesity
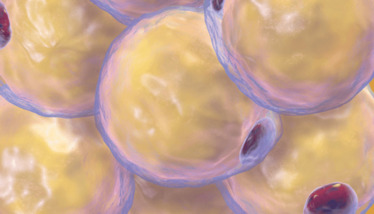
In the hope of treating obesity or type 2 diabetes, researchers from the Joslin Diabetes Center, USA, have used CRISPR to boost expression of the UCP1 gene in progenitor white fat cells to create brown-fat-like cells (1). Brown fat cells are said to be beneficial because they burn energy instead of storing energy, as white fat cells do.
The researchers transplanted their “HUMBLE” progenitor cells into mice on a high fat diet and found that the mice had greater sensitivity to insulin and a greater ability to clear glucose from the blood than the control group. The HUMBLE mice also put on less weight.
Though human trials are still some way off, the team has envisaged an autologous cell therapy protocol whereby a patient's white fat cells are removed, the progenitor cells isolated and modified to boost expression of UCP1, and the resulting HUMBLE cells returned to the patient.
- CH Wang et al., “CRISPR-engineered human brown-like adipocytes prevent diet-induced obesity and ameliorate metabolic syndrome in mice,” Sci Trans Med, 12, 558 (2020). Available at: https://bit.ly/32NqJX1

Over the course of my Biomedical Sciences degree it dawned on me that my goal of becoming a scientist didn’t quite mesh with my lack of affinity for lab work. Thinking on my decision to pursue biology rather than English at age 15 – despite an aptitude for the latter – I realized that science writing was a way to combine what I loved with what I was good at.
From there I set out to gather as much freelancing experience as I could, spending 2 years developing scientific content for International Innovation, before completing an MSc in Science Communication. After gaining invaluable experience in supporting the communications efforts of CERN and IN-PART, I joined Texere – where I am focused on producing consistently engaging, cutting-edge and innovative content for our specialist audiences around the world.



















