Drugs in Disguise
How to dress drugs to help them survive in the bloodstream
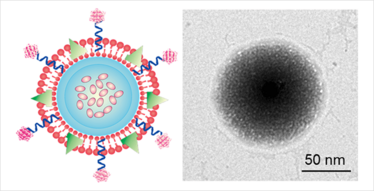
Left: Schematic design of the TRAIL/Dox loaded platelet membrane-coated drug delivery system. Right: A transmission electron microscope image of the drug delivery system; the black part is the synthetic core nanoparticle; the outside shell is the platelet membrane.
A problem with certain cancer drugs is that the body recognizes them as foreign entities and tries to eliminate them, meaning that they don’t survive in the body long enough to be effective. One potential solution is to coat the drug with a cell membrane from the patient’s own cells so that it remains undetected. Zhen Gu, assistant professor at North Carolina State University, and a collaborating research team at the University of North Carolina at Chapel Hill have developed one such drug delivery system that coats a drug with platelets membranes (1).
“The idea was inspired by the relationship between platelets and tumor cells in the body. When a tumor cell separates from its primary tumor site, it enters the blood vessels and begins circulating in the bloodstream. The platelets stick to cancer cells – aided by a specific ligand-receptor recognition (the P-Selectin proteins on the platelet are recognized by the CD44 receptor on the cancer cell) – and the platelet and cancer cell then travel together to a new site to form the metastatic tumor. The platelet helps the cancer cell survive in the bloodstream,” explains Gu.
Recognizing that the platelet interaction could also be exploited to help drugs survive in the body, the team set about creating a platelet-mimicking drug delivery system. “Instead of coating the nanoparticle with multiple proteins expressed on the platelet, we decided that using the whole platelet membrane would be an easy and complete way to generate a platelet-mimicking drug delivery system. We extracted blood from mice, isolated the platelets, then purified and collected the platelet membrane,” says Quanyin Hu, lead author of the paper and a PhD student in the universities’ joint biomedical engineering program.
Two drugs were selected for the study; tumor necrosis factor inducing ligand (TRAIL), and the small-molecule drug – doxorubicin (Dox), although Hu believes that the approach could be applied to any drug. TRAIL was chemically conjugated on the surface of the platelet membrane and Dox was loaded into the synthetic nanoparticle core to create the platelet-drug system. “The transmission electron microscopy displayed the platelet membrane coating as a core-shell structure,” adds Hu. “After being coated with the platelet membrane, the drug can circulate for up to 32 hours, compared to just 6 hours without coating.”
After the platelet-drug comes into contact with a cancer cell, the TRAIL drug is well positioned to attack the membrane. Once internalized by the cancer cells, TRAIL enters the lysosome where the acidic environment breaks down the structure, freeing Dox to do its work.
For now, the approach has only been tested in mice. Gu says, “The next step will be scale-up of the platelet membrane-coated drug delivery system and then testing its efficacy on larger animals. Given the important functions of platelets in several physiologic and pathologic processes, we also want to investigate using the platform to treat other diseases, such as vascular-related diseases and inflammation.”
- Q. Hu et al., Anticancer Platelet-Mimicking Nanovehicles, Advanced Materials, 2015 doi/10.1002/adma.201503323/abstract



















