Derek Gatherer a lecturer at the Faculty of Health & Medicine at Lancaster University, UK, has a deep interest in bioinformatics and believes that viruses are ideal subjects of research. Recently, Gatherer and his collaborators from Aston University, UK, and Universidad Complutense de Madrid, Spain, have designed two universal influenza epitope ensemble vaccines (1). Here, Gatherer tells us more about his interest in influenza and his research.
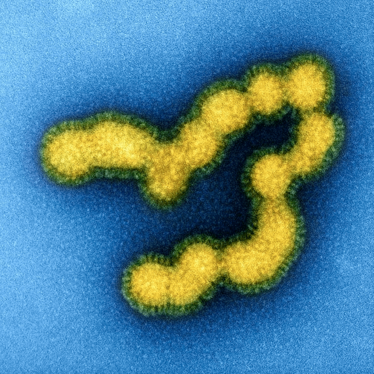
Credit: NIAID
How did you get interested in flu vaccines?
I’ve been interested in flu since the 2009 H1N1 pandemic. My initial interest was mostly in phylogenetics, particularly in the question of flu’s ultimate origins. It’s fairly clear that influenza A is primarily an avian disease – of the 144 subtypes, all but a small handful have been found in birds. Humans have only two subtypes of influenza A currently in circulation: H1N1 and H3N2, and from what we know of them, they clearly show descent from avian ancestors, with some segments passing through pigs on the way to us.
I’ve studied the deeper origins of flu – going back hundreds of years. I’ve noticed that the bifurcations on the tree - the nodes – were not randomly clustered in time. In fact they seemed to be occurring shortly after periods of extreme cold – the so-called Little Ice Ages (LIAs). I developed a theory that LIAs disrupt bird migration, leading to isolated populations in which new subtypes evolve by founder effect. This was published in 2010 (2).
How did this collaboration focusing on the design of a universal flu vaccine begin?
I’ve known Darren Flower, a Research Explorer at Aston University, UK, for over 15 years, but we’ve never managed to work together. He specializes in bioinformatics, computational chemistry and cheminformatics. I was easily persuaded to join the project because I’ve always felt that the current flu vaccination methods, although relatively safe and generally effective, can’t possibly be the best way to go about things.
Past attempts to develop a universal flu vaccine haven’t gone very well. The general principle is obvious – if the HA and NA surface proteins on the flu particle evolve so fast, then why not use something slower moving as a target? And the answer is obvious too – it’s the fact that the immune system mostly reacts to the surface proteins, and that’s why there’s such evolutionary pressure on them. You can choose to immunize with parts of the HA that are further from the surface – the “stalk” approach – or you can choose one or more of the other proteins, but the immune system won’t react as strongly. So the optimal method so far has been to use real viruses – inactivated, of course – as the immunogen. You get the strongest response that way, at the cost of having to refurbish and redistribute the vaccine on an annual basis. The response to a synthetic vaccine may be longer-lasting, but if it’s many times weaker then what’s the point?
You have designed potential universal influenza epitope ensemble vaccines; how?
The first step is the one that has been used in universal vaccine design for the last 30 years or so, which is try to define the conserved regions of the viral genome. There are now thousands of complete sequences of viral genomes, and we have at least one complete from almost every one of the 144 possible subtypes, so we can reliably identify the conserved regions. That gets us as far as all the previous attempts, with the added advantage that there’s enough sequence information in the databases now that we can be a bit more confident about excluding false positives when declaring that certain regions are conserved. The next step is to match this data with what’s in the epitope databases. These are databases of known epitopes – that have been experimentally validated.
We concentrate on CD4+ and CD8+ T cell epitopes. We source these from the Immune Epitope Database and Analysis Resource (http://www.iedb.org/) which has been going for over a decade now and is well curated and maintained. The viral genomes are from the Influenza Research Database (https://www.fludb.org/) and from NCBI’s Influenza Virus Resource (https://www.ncbi.nlm.nih.gov/genomes/FLU/). We finesse the selection of conserved regions in the viral genomes by allowing a little leeway for variation using a Shannon entropy-based technique and BLASTclust and CD-HIT software. We could of course, insist on rigid conservation – but that is potentially vulnerable to disruption by one or two very rare variants. Of course, if we allow too much variation then we risk losing coverage, so it’s a fine balance.
The initial trawl in IEDB produces a lot of output – 210 CD8+ epitopes and 816 CD4+ epitopes. These are influenza A-specific, with an evidential basis. However, a lot of them will be to the variable parts of HA and NA proteins from H1N1 and H3N2 seasonal flus. When they’ve been filtered against our conserved genome regions, the number is reduced significantly.
So having got our epitopes to conserved regions, how do we assess their effectiveness?
This is done using the EPISOPT server (http://bio.med.ucm.es/episopt.html). Each epitope has a population percentage coverage (PPC); for example, among our selected 9 CD8+ epitiopes, it ranges from 1.5 percent to 56 percent coverage (e.g., meaning that 1.5 percent to 56 percent of the population will react). We then combine all PPCs to calculate what proportion of the population would respond to at least one of the epitopes in the cocktail. It turns out that a vaccine needs to have at least six epitope components in order to ensure that 95 percent of the population would respond to at least one of the six. We have two PPC databases to work with, one taken from US data and another from global data, so the calculated cumulative PPCs are different in each case. We have developed two predicted vaccines: one for global use and one for US use. Potentially, each continent or even country, if it had its own epitope PPC database, could derive a locally optimal vaccine.
Finally, we checked back to the flu genomes to see how many different subtypes of influenza had conserved regions. We expected that there would be quite good cross-subtype coverage, but were amazed to see it was as high as 88 percent for the global vaccine and 95 percent in our US-specific vaccine.
What will be the challenges of taking the project further and synthesizing the vaccine?
The major challenge is persuading people who are in principle sceptical concerning universal flu vaccines that ours is different to the others… However, leaving that aside, one of the things that is apparent from our predictive process is that the size of the vaccine is quite large. There are a total of 11 fragments (9 in the US-optimized variant) of total length 117 residues (US-optimized 99 residues) that satisfy our criteria. This is, in a way, quite a welcome find because if each of these produces a weak immune response (as I was saying previously, conservation implies lack of selective pressure, which implies lack of immune pressure), then an individual peptide by itself is not going to be much use as a vaccine. But when we have lots of them, each exerting its own immunogenic effect, the cumulative effect may be more substantial.
But the next question is, how do we deliver this?
One approach is to use a cocktail of synthesized peptides. A second approach is to use a recombinant vaccine, with the peptides embedded in a carrier virus in such a way that they are presented efficiently to the immune system (rather like the Ebola vaccine where the glycoprotein is inserted into an adenovirus delivery system). It could also be possible to use a DNA vaccine approach that relies on the individual’s own cells to synthesize the epitopes. Each has its own advantages and disadvantages. At the moment, we’re still deciding which route we think might be the best option. We also hope to work with lab collaborators who can bring their own opinions to the table.
One further problem is that large parts of the flu genome have been patented! A lot of this is just speculative patenting, designed specifically to cash-in on any future universal vaccines that use the flu genome or peptides made from the flu genome as part of their constituents. Some of the patents are for universal flu vaccines of the past that haven’t (yet) made it to market. This isn’t something that would deter us from pushing on with the project, but it might deter commercial partners. A pharmaceutical company might not want to invest in making something if a potential patent lawsuit is hanging over it.
- QM Sheikh et al., “Towards the knowledge-based design of universal influenza epitope ensemble vaccines”, Bioinformatics, Epub ahead of print (2016). PMID: 27402904.
- D Gatherer, “ The Little Ice Age and the emergence of influenza A”, Medical Hypotheses 75, 359-362 (2010).
Derek Gatherer is Lecturer at Lancaster University, UK.



















