Fighting Flu with Imitation Antibodies
Scientists use computationally designed imitation antibodies to fight the flu – and production costs.
When it comes to the influenza virus, we’re constantly playing catch up – the virus’ frequent mutations necessitate the production of re-formulated vaccines every year, and flu vaccines don’t work well in certain populations, such as the elderly, infants or the immune-compromised.
Not all new antivirals on the market have performed as expected, but scientists believe that monoclonal antibodies (mAbs) could have the potential to broadly neutralize diverse influenzas. However, mAbs have drawbacks: they are costly to produce and require intravenous administration. No wonder then that they have only been developed for severe individual influenza cases within hospital settings.
Now, scientists from the University of Washington want to combine the effectiveness of mAbs with the production costs of antiviral drugs – and are using computationally designed molecules that imitate mAbs to help them in their quest.
In contrast to mAbs (which require hybridoma cell production), the computationally designed molecules – depending on size – can be produced at much lower cost in E. Coli or synthesized without cells, according to the researchers.
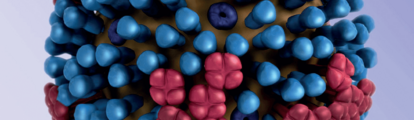
“We have designed a protein that mimics the binding of a potent broadly neutralizing mAb to the HA protein on the surface of the influenza virus,” says Deb Fuller, co-author of a recent study claiming that a single dose of the protein (HB36.6) provided superior protection when compared to 10 doses of Oseltamivir (Tamiflu) against H1N1 virus (1).
The team used computer modeling to design the (HB36.6) antiviral drug. “Most antivirals are discovered by screening natural or synthesized compounds for the ability to neutralize the virus in vitro until you get a hit,” says Fuller. “Computational design is an elegant and more directed approach that focuses on the key interactions known to disrupt the virus, which means there is potential to do ‘one better’ than nature by optimizing those interactions, resulting in an antiviral that binds optimally, with greater affinity to enhance potency.”
Another key finding was that the HB36.6 protein – unlike mAbs and small peptides – could be administered before or after the infection without engaging a host response. “This suggests that HB36.6 could be developed as a superior approach to protect those who are immune compromised, including the elderly, which make up the majority of deaths from seasonal influenza each year,” adds Fuller.
The team also found that when HB36.6 and Oseltamivir were combined, they provided better protection than either alone, suggesting that a flu binder could enhance the effectiveness of flu antivirals currently on the market.
- M.T Koday et al. “A Computationally Designed Hemagglutinin Stem-Binding Protein Provides In Vivo Protection from Influenza Independent of a Host Immune Response”, PLoS Pathog. 4, 12, e1005409 (2016). PMID: 26845438.



















