Preparing for the Next Pandemic
Ever since the “bird flu” outbreaks of the mid-2000s, public health experts have been concerned about an influenza pandemic to rival the 1918 Spanish Flu. Now, blindsided by a less expected beast, can we transfer lessons on pandemic preparedness from flu to COVID-19? We caught up with Russell Basser, Head of R&D at flu vaccine manufacturer Seqirus to find out more about the past, present, and future of vaccine production – and how COVID-19 changes the outlook.
Meet Russell Basser

I started off working at our parent company CSL almost 20 years ago. When the FDA requested that we bring our influenza vaccine from Australia to the US to combat vaccine shortages in the mid-2000s, my group led the clinical and regulatory project. The year 2009 saw the emergence of swine flu, and my group was responsible for supporting the Australian government in their response to the virus.
I found flu a fascinating area and later took on the role of head of R&D for the newly formed Seqirus – a semi-independent business under the CSL umbrella, focusing solely on flu vaccines. My role encompasses everything from basic research through to manufacturing development, clinical, regulatory, drug safety, and medical affairs.
Your company has an interesting origin story…
Commonwealth Serum Laboratories – as it used to be known – was set up by the Australian government in 1916 as a public utility. At that time, it was hard for Australia to get access to modern medicines because they were developed and manufactured such vast distances away. The first big challenge for the newly formed CSL was the 1918–1920 Spanish Flu. The company was successful in producing what was referred to as a vaccine, but was actually an antiserum from patients with pneumococcal infection. CSL went on to produce insulin, penicillin, and vaccines for polio, diphtheria, tetanus, and whooping cough.
The first true vaccines for flu were actually developed in the US in the 1940s, based on the pioneering work of Australian Nobel prize winner Macfarlane Burnet, who discovered that flu could replicate in embryonated chicken eggs. In the late 1950s, CSL brought flu vaccination technology to Australia.
How have manufacturing technologies for flu vaccines evolved since then?
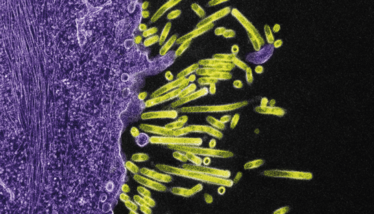
In the early days, the virus was grown in eggs, killed, and injected whole, but this caused some significant side effects. Soon, methods were developed to split the virus using chemical detergents and to purify it to leave only the viral proteins that give maximum immunity and minimum side effects. Even today, up to 90 percent of the world’s flu vaccine supply consists of highly purified, inactivated viruses grown in eggs.
However, egg-based production has some important disadvantages – it’s slow, wasteful, and carries a risk of “egg adaptation” (see sidebar “The Egg (and the Chicken)”). In a bid to develop a faster, more efficient process, Chiron developed a vaccine grown in mammalian cells (dog kidney cells) in the early-2000s. The vaccine was launched in Europe, but it failed to find commercial success when pitted against well-established and inexpensive egg-based vaccines.
The emergence of H5N1 (bird flu) in the mid-2000s brought flu vaccine production into the spotlight. Concerned at the slow turnaround of traditional egg-based manufacturing methods, US government agencies showed renewed interest in cell-based alternatives. With government backing, Chiron (which by this time had been taken over and was, then, Novartis Vaccines) brought the technology from Europe to America, building a new factory in North Carolina – the same factory where we make our cell-based vaccines today. Novartis/Chiron also pioneered the use of an adjuvant called MA59 to boost immune responses to influenza vaccine.
The 2000s also saw the advent of the live attenuated flu virus, administered via a nasal spray (Flumist). Developed by Aviron (later Wyeth, then Medimmune and now AstraZeneca) this frozen vaccine, also produced in eggs, has had something of a chequered history. Initial trials showed it to be highly effective, but logistical challenges hampered uptake. Later, post-marketing data showed that it was not always as protective as hoped, leading to it being dropped from vaccination programs in some countries.
The next big innovation came in the 2010s from Sanofi – a recombinant protein vaccine (Flublok). Insect cells were genetically engineered to produce the most important surface antigen of the flu virus – hemagglutinin. The result is similar to cell culture-based production – faster manufacture and no risk of “egg adaptation.”
Back in the early 2000s, everybody thought flu vaccination was a “dead” area with little hope of innovation. The changes we’ve seen over the past 20 years disprove that – showing that even long-established processes in pharma can be improved upon.
What are the most important lessons the industry has learned from manufacturing flu vaccines over the years?
Around 2005, my boss took a call from the head of CBER, the vaccine division of the FDA. They had just had to close down a major flu vaccine production facility due to quality concerns, which meant there was only one factory licensed to make the flu vaccine for the US market – a precarious position!
How did it come to this? The answer holds an important lesson – not just for flu vaccines, but for medicines more generally. In essence, flu vaccines had become so uneconomical to produce that manufacturers had pulled out. Those that remained struggled financially and started to slip behind in the quality standards demanded by regulatory agencies. When we, as a society, do not value important existing products and focus all our attention on new medicines, we leave ourselves vulnerable.
When H5N1 (bird flu) emerged in the mid-2000s, causing a number of infections in close contact and a mortality rate that suggested it had the potential to cause a pandemic to rival Spanish Flu, the world was less prepared than it could have been. Fortunately, H5N1 has yet to develop the ability to transmit between people but remains a threatening presence in bird populations.
A less severe pandemic emerged in 2009 in the form of H1N1 swine flu, that swept across the globe, causing fatalities amongst children and pregnant women in particular. Since then, governments have been investing more heavily in flu preparedness, in the hopes of being ready for the next pandemic.
What lessons about pandemic preparedness can we take from COVID-19?
We think of our seasonal flu vaccine campaigns as practice runs for a pandemic. We’re very aware that companies like ours are an important line of defence for communities. COVID-19 is, naturally, the overwhelming focus right now, but new flu viruses remain a risk, and there are lessons we can take from COVID-19. One lesson is that days and weeks are very important, and ideally we should be prepared to take action quickly. In many countries, governments were initially slow to take decisive action; the delay has cost many lives.
Another lesson is how important it is to “know your enemy.” SARS-CoV-2 is a new virus but is essentially similar to the viruses that cause SARS and MERS, for which vaccines were already in development before COVID-19 came along. That prior knowledge has enabled rapid development of vaccines for SARS-CoV-2; we already had a good idea of how the virus operates and had an existing target (the “S protein”) that could be rapidly developed into a potential vaccine.
If a new flu virus threatens to take hold, I believe we are in a much better position to respond than we have been to COVID-19, with manufacturing and supply chains already in place around the world. Taking preparedness a step further, Seqirus has already registered a vaccine for H5N1 and gained regulatory approval in the US. If a pandemic were to emerge, we could start manufacturing a vaccine as soon as the genetic code of the strain responsible was sequenced. We believe we could have a vaccine available in as little as three months. We are already in talks with governments about developing similar “pre-pandemic” vaccines for other avian flu viruses, such as H7N9 and H5N6, in case they make the switch to human-human transmission. Over time, we hope to build up a portfolio of these vaccines, ready to roll out if we ever need them.
You can’t be truly prepared until you have tackled something many times. Being prepared “on paper” is a bit like visualizing running fast or kicking a ball into a goal – it helps, but true expertise comes with action. I will remain somewhat cautious about new vaccine platforms until they are truly tested in the field.
Despite your caution, what developments in vaccines are you excited about?
Going back to pandemic preparedness, I believe some of the new technology platforms being developed in the vaccine space are another way in which we can become more responsive to new threats. For example, mRNA and vector-based vaccines could allow very rapid vaccine development. However, these platforms have not been widely used to date and we need more information on safety and efficacy at a population level and over time to confidently rely on these approaches.
Vector-based vaccines, like the SARS-CoV-2 vaccine under development by AstraZeneca and the University of Oxford, are very interesting but, as the vector itself will generate an immune response, they may not be effective if administered more than once or twice.
mRNA vaccines, which get the body itself to produce viral proteins, also have amazing potential. We have an mRNA program at Seqirus and we’ve found that it is possible to generate a new vaccine in a matter of weeks. We’ve also seen very strong responses, even better than many currently commercialized technologies. However, there is much to learn about mRNA vaccines – they seem to cause quite marked reaction at the site of injection, as well as fever when administered at high doses. This latter property indicates that care will need to be taken when administering such a vaccine to young children, who can be especially sensitive to such an effect. Another challenge is that mRNA vaccines are very unstable and have to be frozen. This has been manageable during the development phase, but will add considerable complexity and cost in distribution to the general population, which will provide logistical problems
COVID-19 has brought these new platforms onto the fast-track with almost unlimited money and resources, which could have a positive impact on the field for years to come – and that’s fantastic. But it’s also important to remember that there is still a lot of work to do. As soon as a vaccine shows some success in clinical trials, the press and community at large has expectations that this will make the virus disappear and allow life to return to normal almost instantly. However, population vaccination programs will take time; the first generation of vaccines are unlikely to be perfect and we will continue to learn about their pros and cons along the way.

Is Seqirus involved in SARS-CoV-2 vaccine efforts?
We are partnering with the non-profit Coalition for Epidemic Preparedness Innovations (CEPI) and The University of Queensland (UQ) to help develop their protein subunit vaccine. They are using their molecular clamp platform, designed specifically for rapid response vaccine development. We have provided the MF59 adjuvant, an important additional element that stimulates the body’s immune response to the S protein. The UQ vaccine is currently undergoing phase I trials, and we’ll take responsibility for further development after this study is finished (and assuming it is safe and immunogenic). We have also been contracted to produce the AstraZeneca vector-based vaccine for the Australian Government.
But your main focus remains flu?
That’s right. Seqirus has been an extraordinarily successful industrial experiment! We took unprofitable parts of two companies and created a successful entity, focusing solely on the then-unfashionable area of flu vaccines. The secret of our success has been to keep that focus narrow and deep on the single disease area. Flu is more difficult than most other vaccines, so our laser focus is essential.
There is a saying in the flu world that when you’ve seen one flu season, you’ve seen… one flu season. Every season is different. This is one aspect that distinguishes flu from all other vaccine fields – we’re constantly chasing a mutating virus, but never quite catching up to it. Even with all the advances in medicine, flu remains a challenge. Sometimes the vaccine is very effective, and sometimes the virus drifts after the vaccine strains are chosen and efficacy drops off dramatically.
The deep expertise we’ve developed in flu has allowed us to innovate; in particular, developing the MF59 adjuvant and the cell culture platform I mentioned earlier. Now, we’re combining the two advances. We’ve already done this for our pre-pandemic vaccines, and we hope to soon apply the same combination to create the very best annual vaccine possible with current technology. It’s an exciting direction!
Do you think we’ll ever see a universal flu vaccine?
The press was very hot on this around five years ago and I still get asked about the potential. It is certainly a wonderful prospect: a single vaccine that confers lifelong immunity to all strains of flu. But, as one of my mentors told me, the less you know about something, the more exciting it is. Knowing what I do about the flu virus, I doubt we’ll see a universal vaccine within my working life.
It’s easy to believe fantastic advances like the recombinant HPV vaccines – which require only one dose to provide lifelong immunity – are possible for all viruses. But flu is a different proposition as there are four separate viruses, all mutating rapidly. Before we can even begin to think about a universal vaccine, we need to know a lot more about how the virus behaves in the body and find strategies to trick the immune system into generating a stronger and more long-lived response.
To that end, we participate in a public–private partnership group, the Human Vaccine Project, which is mapping the intricacies of the human immune system down to individual molecules. The aim is to better understand how the body responds to infection and vaccination to see if we can uncover some secrets that might help us generate better vaccines. The exploration is fascinating, exciting and extremely complicated – the more we know, the more we realize we don’t know!
For me, flu is one of the most fascinating spaces to be in. It combines immunology, virology, public health, and geopolitics. And that means it is constantly changing – and constantly challenging.
Russell Basser is Senior Vice President, Research & Development at Seqirus, Australia
The Egg (and the Chicken)
Most flu vaccines are produced in the yolks of fertilized hen’s eggs. It’s a well-established, inexpensive method, but is it still fit for purpose in the 21st Century?
To produce flu vaccines, the WHO has a highly sophisticated surveillance program, with many different labs from around the world submitting samples of flu virus from patients in their area. Based on this information, the WHO makes a twice-yearly recommendation on which strains to include in the vaccine for the forthcoming flu season – once for the northern hemisphere and once for the southern hemisphere.
The chosen strains are then grown in just a few labs worldwide – including Seqirus in Australia, NIBSC in the UK, and the NIH in America. Eggs are not the natural habitat for the flu virus; it must adapt and mutate slightly to grow successfully in this alien environment. For egg-based production, the labs mix the chosen flu strains with a virus that’s known to grow well in eggs and select the mutated virus that represents the best compromise between similarity to the “wild” virus and the ability to grow in eggs. These final strains are then distributed to the flu vaccine manufacturers to produce the flu vaccine for that year.
There is growing evidence that, in certain flu strains, the mutations that allow the virus to grow in eggs can affect the hemagglutinin proteins critical for the efficacy of the vaccine.
Hemagglutinin is the protein responsible for binding to and entering host cells – but the cells in the egg are not the same as human cells, so the protein must alter slightly to be able to reproduce in eggs: “egg adaptation.” And so, when the immune system encounters the wild-type protein, it only partially recognizes it. In years when the dominant flu strain is affected by egg adaptation, egg-based vaccines may be significantly less effective. There are also other challenges associated with egg-based vaccine manufacture. Production is slow (six months), relies on a massive supply of eggs (up to three eggs per dose), and it generates a lot of waste.
Alternatives are available – a vaccine grown in mammalian cells (from Seqirus) and a recombinant vaccine (from Sanofi Pasteur). There is evidence that these egg-free vaccines offer enhanced protection (1), with larger studies underway (2). They are also faster than egg-based methods, offering the hope of a rapid response to any new pandemic strain.
Other companies are looking into a variety of approaches, from growing virus-like particles in plants to mRNA vaccines that cause the body’s own cells to produce flu proteins (3).
Pandemic Century
1918: “Spanish flu”
Cause: H1N1
Global deaths: circa 50 million
1957: “Asian flu”
Cause: H2N2
Global deaths: circa 1.1 million
1968: “Hong Kong flu”
Cause: H3N2
Global deaths: circa 1 million
2009: “Swine flu”
Cause: (H1N1)pdm09 virus
Global deaths: circa 284,000
2019: COVID-19
Cause: SARS-CoV-2
Global deaths as of November 2020: 1.23 million
- LM Dunkle et al., “Efficacy of Recombinant Influenza Vaccine in Adults 50 Years of Age or Older,” The New England Journal of Medicine, 376, 2427-2436 (2017).
- ClinicalTrials.gov, “A Pragmatic Assessment of Influenza Vaccine Effectiveness in the DoD (PAIVED),” (2018). Available at bit.ly/37qofBL.
- Nature, “Accelerating flu protection,” (2019). Available at go.nature.com/3dJKq7b.

Making great scientific magazines isn’t just about delivering knowledge and high quality content; it’s also about packaging these in the right words to ensure that someone is truly inspired by a topic. My passion is ensuring that our authors’ expertise is presented as a seamless and enjoyable reading experience, whether in print, in digital or on social media. I’ve spent fourteen years writing and editing features for scientific and manufacturing publications, and in making this content engaging and accessible without sacrificing its scientific integrity. There is nothing better than a magazine with great content that feels great to read.



















