The Four Most Promising Adoptive Cell Therapies
A whistle-stop tour of the mechanisms, benefits, manufacturing challenges, and clinical potential of CAR T cells, TCR T cells, TILs, and NK cells
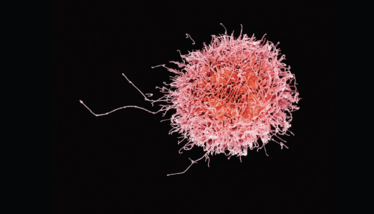
Credit : NIAID/Flickr.com
For far too long, patients with cancer had access to only a few treatment options – and none were ideal. Surgery is invasive and risky, while radiation and chemotherapy are toxic and offer variable success rates. In the last decade, however, thanks to advances in increased understanding of genetics and the immune system, researchers have developed more personalized, targeted therapies that promise better outcomes for cancer patients. Immunotherapy, including adoptive cell therapy, defines a new generation of cancer treatments that could drastically change clinical strategies and outcomes.
Here, I review the mechanisms, benefits, manufacturing challenges, and clinical potential of the four most promising types of adoptive cell therapies: chimeric antigen receptor (CAR) T cells, T cell receptor (TCR) T cells, tumor infiltrating lymphocytes (TILs), and natural killer (NK) cells.
Our biological watchdog
The core purpose of the immune system is to discriminate between “self” and “non-self” and destroy anything that does not belong. The human immune system identifies pathogens ranging from bacteria to viruses and activates lymphocytes, such as T cells and B cells, to attack them. However, the immune system struggles to recognize tumors, which can often grow rapidly and spread unchecked throughout the body.
Adoptive cell therapy, also called cellular immunotherapy, uses immune cells to treat cancer. As of 2021, only one type of adoptive cell therapy has received approval from the FDA: CAR T cell therapy. The first approved CAR T cell therapy treats acute lymphoblastic leukemia. Today, there are five CAR T therapies on the market, treating a range of blood cancers, including multiple myeloma and mantle cell lymphoma.
However, other types of adoptive cell therapies are now in advanced stages of development and are likely to enter the clinic soon. Tumor infiltrating lymphocytes (TILs), for example, are on the verge of approval, having already received a breakthrough designation for treating advanced cervical cancer and an orphan drug designation for advanced melanoma (Iovance’s LN-145 and Instil Bio’s ITIL-168, respectively). T cell receptor (TCR) T cells have also shown promise in the laboratory but have not yet reached the clinic – and the same is true for natural killer (NK) cells.
Though promising, no one type of adoptive cell therapy is perfect. These therapies are challenging to develop and manufacture efficiently, and it is difficult to predict how individual patients will respond to treatment. In addition, each therapeutic approach offers distinct benefits and harbors specific limitations.
CAR Ts
CAR T cells have demonstrated incredible success in the clinic. Engineered to express the chimeric antigen receptor (CAR) protein, CAR T cells seek out tumor cells that express certain surface markers and destroy them. In a way, CAR T cells recognize tumor cells as infectious agents.
Today’s approved CAR T cell therapies are autologous, meaning they are derived from a patient’s own T cells. This process offers safety benefits for patients but also poses a manufacturing problem. To develop CAR T cells, a patient has their blood drawn, and then the blood is sent to a laboratory, where scientists extract the T cells and genetically engineer them using viral vectors or transposon systems to express the CAR protein. Next, they expand the cells and return them to the clinic, where a physician infuses the patient’s modified T cells back into their body. Since the cells originally came from the patient, the chance of the patient experiencing an immune reaction to the cells is minimal.
But autologous CAR T cells are hard to manufacture efficiently. The process often takes weeks – time that patients may not be able to afford. To address this issue, scientists are developing allogeneic CAR T cells that could be manufactured in advance and administered “off the shelf.” This option poses a different set of pros and cons: while allogeneic CAR T cells could potentially reach patients in days instead of weeks, their foreign nature puts patients at risk of either contracting graft-versus-host disease or seeing their immune system kill off the transfused cells before they can have an effect.

Author: Marwan Alsarraj is the Biopharma Segment Manager at Bio-Rad.
As T cells are complex living cells, CAR T cell manufacturing and development requires rigorous quality control. Biomanufacturers cannot entirely predict how the cells will act either in vitro or in vivo. Therefore, they cannot predict the success of the cells’ development or application in the clinic. For instance, viral transduction of the CAR transgene is not guaranteed, and variations in copy number can lead to varying clinical success: if transduction is not successful, the treatment won’t work, and if the copy number is too high, the treatment can become toxic. Furthermore, the cells could potentially contain replication-competent viruses that can infect patients. Finally, researchers cannot always predict how long CAR-T cells will persist once administered to patients, so they must conduct serial monitoring to assess the ongoing viability of the treatment.
New technologies can help in this regard. As one example, droplet digital PCR (ddPCR), which detects rare nucleotide variants and quantifies them directly, can be used to assess the quality of CAR T cells. ddPCR can quantify nucleic acids down to one copy per genome, qualifying it as technology suitable for serial monitoring of CAR T persistence in the blood.
All current FDA-approved CAR T cells treat blood cancers, as the CAR T cells in use today cannot infiltrate solid tumors. However, scientists are starting to identify novel targets that will enable CAR T cells to attack solid tumors.
More than 630 CAR T cell trials are registered on ClinicalTrials.gov as either recruiting or ongoing. By 2028, the market may reach $8 billion in size (1).
T Cell Receptors
Like CAR T cell therapy, TCR therapy involves genetically modifying T cells, yet the two therapies work via different mechanisms. CAR T cells target specific antigens present on the surface of cells, which explains why they struggle to infiltrate solid tumors. In contrast, TCRs can target any antigen, whether it is present on the cell surface or within the cell, suggesting that this therapy might be applicable to other types of cancer (2). TCR T cells bind to a cell’s major histocompatibility complexes (MHCs), the innate immune system’s protein structures that tag cells for destruction, thereby enhancing the body’s natural immune response.
Like CAR T cells, TCR T cells are personalized to each patient, slowing down the development process and delaying treatment. As researchers continue to study the feasibility of developing allogeneic CAR T cells, TCR T cell development should benefit, as well, creating two viable forms of T cell mediated therapy.
TCR T cells are running behind CAR T cell therapies in development, but around 280 TCR clinical trials are recruiting or ongoing, according to ClinicalTrials.gov.
Tumor Infiltrating Lymphocytes
Lymphocytes that successfully enter tumor tissue are called TILs – and scientists are looking to exploit this ability to treat cancers that are off-limits to current CAR T cells. Unlike CAR T and TCR T cells, TILs do not need to be genetically modified. Since they specifically infiltrate tumors, they already recognize all the antigens needed to fulfill their intended purpose. Instead, these cells merely need to be expanded ex vivo to enhance their effect within the body.
But this expansion process is not simple, making the cells difficult to scale up for commercial use. While T cells can be harvested via a blood draw, TILs can only be collected after resecting tumor tissue from a patient. The tissue needs to be dissected, plated, and digested to isolate the T cells. Finally, the cells get expanded and returned to the patient. From biopsy to reinfusion, the process takes about six to eight weeks and requires significant technical skill. This convoluted process might explain why, despite over 20 years of research, this therapy has not yet reached the clinic. Unsurprisingly, researchers are investigating new methods to simplify the development process.
Despite the hurdles, about 300 clinical trials for TILs are currently enrolling or active on ClinicalTrials.gov.
Natural Killers
Unlike the first three adoptive cell therapies, NK cell therapy does not involve T cells; NK cells are a different type of lymphocyte that specifically targets tumor cells, granting them unique therapeutic potential. NK cells do not need to be genetically modified to identify tumors or any specific antigen on tumor cells. Instead, they attack tumor cells directly and release chemokines and cytokines that activate the adaptive immune system.
NK cells do not sufficiently kill off cancer cells on their own because tumors release inhibitory molecules that suppress their activity (3). However, activating them ex vivo, expanding them, and modifying them to express the CAR protein could help them overcome inhibition and kill tumor cells (4).
Allogeneic, unmodified NK cells are safe, indicating that they could potentially be standardized and offered off-the-shelf (5). But manufacturers still have several hurdles to overcome to make the approach viable for clinical use; for example, it is difficult to expand NK cells in vitro and they also struggle to infiltrate tumor tissue, meaning they might not be suitable for use against solid tumors. They also do not persist in the blood for as long as CAR-T cells. But given NK cells’ natural ability to target tumor cells, scientists are optimistic about their therapeutic potential. After further research and development, these could become cheaper, easier to produce, and more widely available than CAR T cells (6).
Over 300 NK cell trials are currently enrolling patients or ongoing for people with cancer on ClinicalTrials.gov – and forecasters expect the market to reach $5 billion by 2026 (7).
Making a difference
Together, these four adoptive cell therapies could give many people with cancer a chance to live a better, longer life. Though they all present unique development challenges, hundreds of clinical trials are underway to investigate their therapeutic potential. The science will continue to advance as researchers discover how lymphocytes interact with tumor cells and as the field refines genetic engineering and ex vivo expansion protocols. With this additional knowledge, it will become easier to produce these “living drugs” effectively.
The FDA supports the development of adoptive cell therapies and understands the challenges inherent in developing them – and that’s why the agency has released several guidelines on cell therapy manufacturing (8). Through the combined efforts of academic researchers, biopharmaceutical companies, and regulators, these four adoptive cell therapies could reach their clinical potential and make a significant difference in patient outcomes.
- Coherent Market Insights, “Global CAR-T Cell Therapy Market to be Worth US$ 8 Billion by 2028” (2018). Available at: https://bit.ly/3c0hKqq
- Arnaud M et al., Front Immunol 12, 701636 (2021). DOI: 10.3389/fimmu.2021.701636
- Cózar et al., Cancer Discov, 11, 34–44 (2021). DOI: 10.1158/2159-8290.CD-20-0655
- Shimasaki N et al., Nat Rev Drug Discov, 19, 200–218 (2020). DOI: 10.1038/s41573-019-0052-1
- Liu S et al, J Hematol Oncol, 14, 7 (2021). DOI: 10.1186/s13045-020-01014-w
- Senthil P et al., J Young Investigators, (2020). DOI: 10.22186/jyi.38.5.36-42
- Allied Market Research, “Natural Killer Cells Therapeutics Market by Therapeutics (NK Cell Therapies and NK Cell Directed Antibodies), Application (Cancer, Gastrointestinal Diseases, Immunoproliferative Disorders, and Others), and End User (Research Centers & Institutes, Hospitals, and Others): Global Opportunity Analysis and Industry Forecast, 2018–2026,” (2019). Available at: https://bit.ly/3oqo4xs
- FDA, “Cellular & Gene Therapy Guidances,” (2021). Available at: https://bit.ly/3D2ouQx
Marwan Alsarraj is the Biopharma Segment Manager at Bio-Rad. He has been at the forefront of developing, marketing, and commercializing technologies in the past 15 years in the life science research industry. Marwan obtained his MS in Biology at the University of Texas, El Paso.



















