
The mRNA Manufacturing Advantage
COVID-19 vaccine success has proven the many benefits of mRNA. With mRNA offering more straightforward development, simpler manufacturing processes, and smaller facility footprints, are the days of traditional vaccine modalities numbered?
Natraj Ram |
sponsored by Thermo Fisher Scientific
Within weeks of identifying the SARS-CoV-2 virus, scientists in China had determined its structure and published the information in the public domain. Immediately, scientists began working on vaccine designs and, within a matter of weeks, vaccines were undergoing early testing. Just eleven months after the discovery of SARS- CoV-2, regulators in the UK granted emergency-use authorization for not only the first COVID-19 vaccine, but also the first mRNA-based vaccine. It was a historic moment.
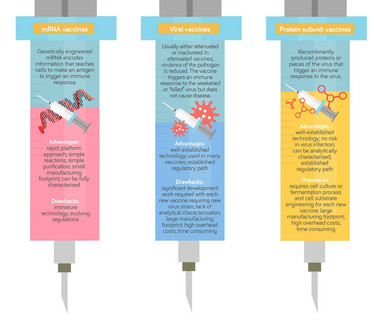
The drawbacks of tradition
Traditional vaccine approaches have worked well. Collectively, vaccines have arguably done more good for humanity than any other medical advance. However, they are costly, time-consuming, and slow to develop. Most vaccines are viral based, using attenuated or inactivated versions of the target virus. Examples for viral-based vaccines include ProQuadTM for measles, mumps, rubella, and varicella; RotaTeqTM for rotavirus, AvaximTM for hepatitis A, and many flu vaccines (including FluzoneTM, FluLavalTM, and FluadTM).
However, growing and subsequently weakening or inactivating the viruses requires significant time and money. When scaling up, close attention must be paid to selecting systems able to produce large quantities of a target virus safely, robustly, and as economically as possible. With live attenuated viruses, there is a low frequency of reversion to virulence. This is particularly problematic for viruses such as dengue, for which there are four serotypes, as antibody- dependent enhancement (ADE) is known to occur, and neutralizing antibodies for all four serotypes are necessary to confer protection.
Non-viral vaccines have also been developed, including virus-like particle (VLP) vaccines such as GardasilTM (Merck & Co.’s HPV vaccine), conjugate vaccines such as PrevnarTM (Pfizer’s pneumococcal vaccine) and recombinant protein vaccines such as ShingrixTM (GSK’s herpes zoster vaccine). Each of these different vaccine types has its own challenges during development. Developers first need to identify the antigen that will trigger a sufficiently robust immune response to obtain protection, demonstrate safety and efficacy during clinical trials, and develop a robust process for manufacturing. These activities are time-consuming and expensive, and even decades of investment do not guarantee successes.
mRNA: a platform for success
To put it bluntly, traditional vaccines take a long time to commercialize. The level of difficulty in both developing and testing new vaccines remains a high hurdle for any biotech or pharma company to jump. Even the duration of early clinical trials can be daunting. Clearly, the clinical testing designs and requirements are still the same for mRNA vaccines, but the development time is significantly shor ter because there are less complicated steps to address; for example, as mRNA vaccines do not use viruses, there are no potential safety issues associated with virus particulates. The purification process is also easier. Finally, the mRNA approach avoids the lengthy use of cell cultures and the optimization required to achieve the right growth conditions.
In short, the overall development and manufacturing process for mRNA vaccines is much faster. Once you have the template DNA, the mRNA process relies on in vitro transcription (IVT) and purifications. IVT techniques have been in place for many years now; the challenge over the course of the pandemic has been to bring these up to an appropriate scale.
Indeed, scale has been a major differentiating factor for traditional and mRNA vaccine approaches. If you need to make enough doses to vaccinate the global population, a traditional viral- based system may require hundreds of thousands of liters of bioreactor volume to produce 20 million doses per month- resulting in the need for large facilities and high overhead costs. The same 20 million doses per month can be produced in a single 30 L mRNA IVT system. Multiple mRNA systems can be set up in a small footprint or small facility quickly and efficiently; moreover, various vaccine targets can be run in parallel. Since mRNA works as a platform process, you only need to change your DNA template for each new vaccine — the rest of the process remains the same. In contrast, with a live virus, every new vaccine requires a new virus strain and potentially a new cell line.
One further advantage with mRNA vaccines is that analytical characterization is much easier. mRNA is amenable to rapid testing for consistency throughout the various purification steps, giving manufacturers the opportunity to really understand both the process and the product. For some viral-based vaccines, such as RotaTeqTM (Merck & Co.’s rotavirus vaccine), it is impossible to fully characterize the end product.
But that is not to say an mRNA vaccine is easy to develop — specific expertise is still required. mRNA must reside inside lipid nanoparticles that can pass from the injection site to the immune system while preventing the vaccine from being destroyed in the blood. The delivery system must be carefully tailored, and the RNA sequence must be modified to prevent severe immune system reactions and to educate the immune system properly.
Enabling with options
Perhaps the biggest hurdles for any new therapeutics approach are gaining regulatory confidence from successful trials and establishing credibility with the wider population, including patients. COVID-19 mRNA vaccines jumped these hurdles at high speed. Excitingly for the future, the effectiveness of mRNA-based vaccines has been proven on a massive scale, and this exposure and public acceptance will promote their application in other therapeutics solutions.
At the same time, as mRNA is a new field, no one yet has all the puzzle pieces. Even with the established technologies available, there is still room for improvement and optimization. Thinking of global accessibility, the next industry challenges that need to be addressed are material costs and drug product stability. Here, partnerships between drug developers and suppliers will be critical.
At Thermo Fisher Scientific, we want to be part of this partnership and we are working hard on the next generation of technologies that will help improve workflow efficiencies and bring down total costs. By continually developing and introducing new products, including analytical equipment, production tools, and raw materials, we are helping to remove process and workflow limitations, enabling developers to optimize based on the specific nature of their mRNA production and purification processes. For any vaccine developer looking to thrive in this new space, selecting the best options to meet technical challenges will accelerate the path to commercialization.
Vice President of Innovation, Bioproduction, Thermo Fisher Scientific



















