Zero Defects
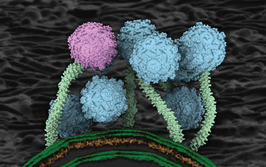
Lives and livelihoods depend on accelerating large molecule drug production, so biopharma companies must minimize defects and contamination
Massimo Mainetti | | Opinion

As the COVID-19 pandemic continues to unfold, the industry is working tirelessly to identify effective treatments and vaccines. There is intense pressure to produce a vaccine in a short time frame, which demands efficiency on all fronts. Naturally, large molecules are being considered as treatments, but manufacturers face the challenge of ensuring that such drugs have zero defects and do not contain silicone contamination from packaging and delivery. Although silicone contamination has been an issue for decades, it can be commonly found in the plungers and stoppers of syringes, cartridges and vials. Because of its ubiquity, the default tendency among pharmaceutical and biotech manufacturers is to “work around” the possibility of silicone contamination in drug formulation, rather than address the issue head-on. Such contamination challenges are surmountable; indeed, solutions in this space can save pharmaceutical companies time, money and stress, while delivering a better product to the patients.
When producing parenteral packaging for vulnerable or sensitive products, such as large molecule drugs, medicine manufacturers should always aim for zero defects. The zero-defect approach better preserves the drug, protects the patient, and upholds the reputation of the drug manufacturer. Injectable biologics have emerged as chief drivers of sales growth in the pharmaceutical industry, but are costly to manufacture and often highly sensitive to extraneous contamination, such as silicone, cellulose, or other particles. If the drug includes unsatisfactory levels of any of these contaminants, the whole batch must be disposed of, representing a significant monetary loss and, as we are reminded amid today’s pandemic, precious time wasted in moments of potential crisis. Despite all the industry-standard quality audits and third-party oversight, contamination of large molecule drugs is still commonplace.
What best practices reduce incidence of drug contamination? In the case of silicone in parenteral drug packaging, it can start with complete coverage of any plunger or stopper with a no-silicone fluoropolymer coating. Creating a robust barrier between the drug and rubber minimizes the impact posed by extractables and leachables. Additionally, drug and device manufacturers can seek ready-to-use components in rapid transfer port (RTP) bags, so that drug manufacturers do not have to sterilize their own components. Pushing the washing and sterilization of components further upstream to component manufacturers reduces the manufacturing footprint in a biologics facility, and also keeps the focus on the core competency of manufacturing and filling the drug product rather than on component processing – which itself requires meticulous attention to detail.
Another best practice is to establish clear, transparent channels of communication between key parties – the drug company, the packaging manufacturer, and other essential suppliers. By working more closely, specifiers can easily identify and troubleshoot potential sources of contaminants and eliminate common defects throughout the supply chain; a crucial endeavour when you consider that visible particles accounted for 22 percent of all injectable drug recalls between 2008 and 2012, and that recall events due to visible particulates have been steadily increasing since 2009. Component manufacturers should consider redesigning production facilities for packaging and delivery systems used in large molecule drug applications to eliminate the presence of identified contaminants. Packaging production facilities should be designed to meet the highest manufacturing standards such that they serve as an extension of the API manufacturing environment.
Perhaps the most common contaminants in pharmaceuticals are cellulose (cotton and paper) fibers, synthetic fibers, silicone, plastics, rubber, metal particles and corrosion products, glass particles and vial delamination flakes, skin flakes, and char particles. Eliminating cellulose from the vicinity of production is particularly difficult. Cellulose can be introduced via wood pallets, paper and bags present near production environments. Eliminating paper from the production floor – and, if possible, in the surrounding offices and other areas – by transitioning a facility to all electronic records and communications, can go a long way to reducing cellulose particles that can circulate. Substituting wood pallets with non-contaminating versions made of plastic substrate is also recommended.
Finally, it’s necessary to improve product inspection. Camera inspection adds a layer of security the naked eye cannot achieve alone. Cameras do not get tired and do not miss even the smallest anomaly. For regulators, the trend is toward increased stringency. Consequently, drug manufacturers and the designers of packaging and secondary devices are under increasing levels of scrutiny. Recently, the FDA set the bar even higher for injectable drug manufacturing by calling for implementation of improved specifications, increased inspection, and improvement in analytical and inspection techniques (1).
Meanwhile, the creators and end users of large molecule drugs are relying on parenteral drug packaging companies to get as close to zero defects as possible. Anytime there is a market recall, it is not just a financial liability, but a huge risk to the reputation of pharmaceutical company partners and to the health of waiting patients.
The harsh reality? Contamination will always be an issue, and so “zero defects” represents a truly aspirational or idealistic goal; we in the industry must tackle this engineering challenge head on so that we can at least get as close as possible.
- FDA, “Statement from FDA Commissioner Scott Gottlieb, M.D., on new steps to strengthen and modernize agency’s oversight and reporting of inspections for sterile injectable drugs,” (2018). Available at bit.ly/3f5zZuu.