A Call for Cell Support
Engineered cell therapies hold exciting potential for the pharmaceutical industry – but only if contract manufacturing organizations and vendors play their part in the revolution.

I’ve always been someone who enjoys bringing new treatment options to patients, particularly those with unmet medical needs. For much of my career, I’ve focused on developing monoclonal antibodies for auto-immune diseases, but today I work with cell therapies – an incredibly exciting area. The technology is certainly new, but it has great potential. In fact, you could say that we are on the cusp of an industry revolution – the cell therapy revolution.
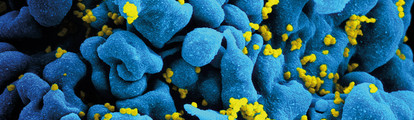
The potential of cell therapies – the use of living cells to treat disease by replacing damaged or missing cells – comes at a cost; it adds layers of complexity to the drug development process not seen with traditional small- or even large-molecule drugs. I describe cell therapies as a three-dimensional approach because of their multiple mechanisms of action. Small-molecule drugs are generally simple with a one-dimensional way of working, since they tend to act on specific molecular targets. When we move onto biologic medicines, we are working with more complicated molecules that make it more difficult to define the product since they can work in many ways and have unexpected effects. With a cell therapy, the complexity increases even more but it also produces opportunities – the therapeutic agent in question is a living organism, able to sense and assess its surroundings, and react and deliver effects through multiple mechanisms of action.
Our current focus is on T cell engineering. But all of the ongoing research into cell therapies can only benefit patients if we can solve the manufacturing challenges too. Here, as well as highlighting some of our research, I’d like to focus on the manufacturing hurdles. In particular, we need to find new business and manufacturing models that suit these therapies – and we need contract manufacturing organizations (CMOs) and equipment suppliers to help us along the way.
Engineering living agents
Much of the hype around cell therapies centers on the potential of cell engineering. Cells are live agents and they are very powerful – able to carry out functions that we can’t accomplish with small- or large-molecule drugs. If we can harness cells as cell therapies and program and direct them using cellular engineering, then we have the power to moderate and direct therapeutic effects – with virtually unlimited opportunities. We’ve seen this with the CAR-T approach in oncology, which involves engineering patients’ own immune cells to attack their tumors. Only a few trials have been done so far, but the results have been promising.
Engineering cell therapies could also be used to tackle other therapeutic areas – I’ve mainly focused on autoimmune and chronic inflammatory diseases. My company holds several patents on regulatory T cells (Tregs) – naturally occurring blood cells that help induce tolerance against foreign antigens taken up by inhalation or ingestion, for example. Their role in the body is to control inflammation using various mechanisms of action through proliferation including pro-inflammatory cell inactivation and cytokine production. Our research has shown that they may hold therapeutic potential in a number of autoimmune and chronic inflammatory diseases in different experimental animal models. Our founder was involved in the discovery of these cells in 1997, and much of our work has centered on translating their therapeutic properties into actual medicines.
One approach is priming Treg cells to specifically recognize an antigen present at the site of inflammation. The chosen antigen then triggers Treg activation locally in the inflamed tissue, resulting in local immunosuppression. We’re working on a manufacturing process that involves using a single blood sample from a patient, educating the cells ex-vivo to specifically recognize a chosen antigen, and then mass producing and freezing the cells, which will be administered to the patient via injection. When the patient’s own Treg cells are re-injected, they target the site of inflammation. Following success with antigen targeting, we are now developing engineered Tregs with the ability to deliver their immunomodulatory action independently of traditional antigen presentation using chimeric antigen receptors. This approach is very inspiring because, with genetic engineering, we have the opportunity to meet an even wider spectrum of chronic inflammatory and autoimmune conditions compared to antigen targeting alone.
Manufacturing models
As noted, although early studies have demonstrated the potential of engineered cell therapy, there is a large hurdle to overcome in bringing such therapies to patients. We must consider the challenges of producing and selling cell therapies on an industrial scale.
Cell therapy manufacture is currently specialized and expensive – and tends to involve slow, manual processes. We need to move to a business model that will allow us to more easily bring large batches of cell therapy to patients at an acceptable cost. Even in the early stages of cell therapy research and development, companies need to start thinking about their target patient population, expected capacity needs, and how they will reach the market. In some cases, it will be better to use CMOs than to build a new facility – which is the route we’re taking at TxCell; we’ve partnered with a CMO in Belgium. Outsourcing is commonplace with traditional small molecules and biologics, but when it comes to cell therapies it is a little more difficult to simply hand these products over. Very few CMOs can handle cell therapies, but capacity and knowledge is growing. In the future, I expect to see – and we certainly need – significantly more CMOs that are able to cope with cell therapies.
As well as a lack of CMOs, there is also a lack of suitable equipment. Contamination is a particular problem for cell therapy manufacturers due to the challenges of working with live products – and the fact that the final therapy cannot be terminally sterilized at the end. Correctly sizing manufacturing setups and automating line manufacturing will prevent congestion problems, which will also help prevent contamination down the line. But developing closed systems, whereby all samples are isolated, is key to preventing contamination. Unfortunately, few automated technological solutions exist that can aid in cell therapy manufacture at all – let alone closed solutions. But if we have a vision of where we want to go as an industry, then the technical solutions will emerge. We’ve seen this happen before in biologics – the boom in bioreactors and other equipment for biomanufacturing didn’t happen overnight, but it did happen. Five years ago, there were few companies contributing to the cell therapy area in terms of coming up with technical solutions for manufacturing. Now, I see more companies working on this. At the moment, we often seem to be seeking solutions that don’t exist… But given the real and growing need, there is a clear business opportunity – and that means innovation will come.
The challenges of cell therapies are certainly significant – but we scientists love challenges that make things interesting, don’t we? I really believe that cell engineering will transform cell therapies and the field of medicine. In the future, we may be able to engineer biological robots – cells that can precisely target certain sites within the body to deliver specific effects. These therapies do not fit into traditional business or manufacturing models so companies will need to have the courage to take risks and to try out new things. I think that the pharma industry as a whole tends to be very risk-averse, but as we see more cell therapy successes, I believe more activity and established business models will begin to emerge.
We’re already seeing a rise in cell therapy applications in oncology and it will spread to other fields too. But rather than waiting and following the crowd, companies that want to get involved in cell manufacturing must start preparing for the future and trying out new strategies. At TxCell, we’ve carefully defined our product profiles, as well as how manufacture will evolve and how the product will be used. Other companies should be doing the same.
Miguel Forte is SVP, Chief Operating Officer, at TxCell.
Cell Successes
Oncology
Chimeric antigen-receptor (CAR) T-cell therapy involves harvesting T lymphocytes from patients, modifying them in vitro to recognize malignant cancer cells and then infusing them back into patients. It has generated a lot of excitementation in oncology and in December 2014, scientists reported that a Phase I trial examining the potential of a CAR T-cell therapy to treat refractive acute lymphoblastic leukemia saw remission in 24 out of 27 patients (1).
More CAR T-cell therapies are now being trialed by a number of companies and research institutes, with some studies also focusing on solid tumors.
Ophthalmology
In early 2015, the European Medicines Agency recommended Holoclar (manufactured by Holostem Terapie Avanzate) – a stem cell therapy used to replace cells on the cornea that have been damaged by burns – for approval in the EU (2). The treatment involves taking limbal stem cells from the eye’s limbus, growing them in the lab, and transplanting the cells back into the eye to repair the cornea after injury. This is the first stem cell therapy to receive regulatory approval in the Western world.
Stem cells have also been investigated as a treatment for macular degeneration with a number of trials taking place. For example, in September 2015, a trial for wet macular degeneration was initiated in the UK at Moorfield’s Eye Hospital (3).
Heart regeneration
In October 2015, Cell Therapy Ltd began the application process for a conditional marketing authorization in Europe for Heartcel – an allogeneic stem cell therapy to regenerate areas of the human heart damaged by heart attack or heart failure (4). Filing is planned for mid-2016 and the company has already had a pre-submission meeting with the European Medicines Agency.
Diabetes
In 2015, ViaCyte’s stem cell-derived, encapsulated cell replacement therapy for type 1 diabetes began a Phase I clinical trial (5). VC-01 cells are implanted under the skin of the patient; the cells then differentiate to produce mature pancreatic cells that synthesize and secrete insulin.
- C.J. Turtle et al., “Acute Lymphoblastic Leukemia: Therapy, excluding Transplantation: Immunotherapeutic Trials in ALL,” 56th ASH Annual Meeting and Exposition (December 2014).
- EMA, “First stem-cell therapy recommended for approval in EU,” (December, 2014).
- Moorfield’s Eye Hospital, “New trial for wet AMD,” (September, 2015).
- Cell Therapy Ltd, “Cell Therapy Ltd to submit Heartcel for conditional marketing authorisation post meeting with the European Medicines Agency,” (October 2015).
- ViaCyte, “ViaCyte Receives Clearance from Health Canada for Diabetes Clinical Trial” (January, 2015).



















